Additive Manufacturing of Medical Implants: A Review
E. Gordon
Wayne State University College of Engineering
Abstract
Additive manufacturing has numerous applications and is gaining interest in the biomedical field. The quality of additively manufactured parts is constantly improving, which contributes to their increased use for medical implants in patients. This paper reviews the literature on surgical additive manufacturing applications used on patients, with a focus on the customization of 3D printed implants and the ability to incorporate scaffolds on the implant surface. Scholarly literature databases were used to find general information on the focus topics, as well as case studies of surgical applications of additive manufacturing implants in rodents and humans. The advantages of additive manufacturing medical implants include improved medical outcome, cost effectiveness, and reduced surgery time, as well as customization and incorporated scaffold. Overall, the most effective type of additive manufacturing for the medical implant application is electron beam melting using Ti-6Al-4V because it can produce a high quality, high purity biocompatible implant that has the required mechanical properties.
Keywords: Additive Manufacturing, Customized implants, Scaffold, 3D Printing, Ti-6Al-4V
Introduction
In recent years, additive manufacturing technologies have improved significantly, thus expanding the fields and applications for which they can be used. These 3D printing technologies create physical models from digital models without the need for tool and die and process planning. Additive manufacturing can fabricate prototypes of complex shapes in a variety of materials such as metals, polymers, and nylon. Metal components, in particular, can be used for practical applications such as medical implants: devices manufactured to replace or support a biological structure. The biocompatibility of these metallic devices must be considered, creating rigorous requirements for the material selection and final material properties of the structure. Studies have shown that additive manufacturing successfully produces implants with biocompatible materials that meet the structural requirements [1-6].
3D printing medical implants can provide many benefits such as the customization and personalization of the implants, cost-effectiveness, increased productivity, and the ability to incorporate scaffold. Using custom made implants, fixtures and surgical tools can help decrease surgery time and patient recovery time, while increasing the likelihood of a successful surgery [7]. Another benefit is the cost efficiency of 3D printing medial implants. Traditional manufacturing methods are cheaper for large quantities, but are more expensive for personalized designs and small production runs [8, 9]. 3D printing is especially cost effective for small-sized implants like spinal or dental implants. 3D printing is also faster than traditional manufacturing if a custom implant needs to be made; traditional methods require milling, forging, and a long delivery time while 3D printing may only take about a day [1]. Another notable benefit of additive manufacturing is the ability to share data files of designs. Files saved as an .STL can be downloaded and printed anywhere in the world. The National Institutes of Health established a 3D Print Exchange to promote open-source sharing of 3D print files for medical models [7]. The most significant benefits for the biomedical industry, however, are the ability to manufacture biocompatible materials, customize implants, and incorporate a porous scaffold surface.
Types of Additive Manufacturing
The additive manufacturing approach uses computer software to slice a complex 3D model into layers of 2D cross-sections with a minute thickness. The layers are then printed layer by layer depending on the particular method chosen for the application. There are dozens of types of additive manufacturing systems on the market, some of the most common being stereolithography (SLA), direct metal laser sintering (DMLS), selective laser sintering (SLS), selective laser melting (SLM), 3D printing (3DP), and electron beam melting (EBM). These systems are classified according to the form of the raw material, which can be powder, liquid, or solid form [8]. The two types of additive manufacturing that are most commonly used for medical implants are SLS and EBM.
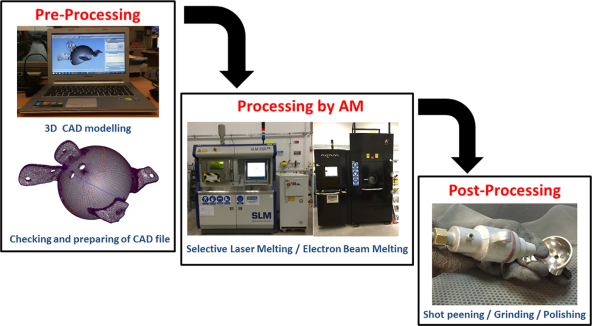
Figure 1: Process chain for SLM and EBM. The pre-processing before manufacturing includes 3D modeling, file preparation, and slicing of the 3D model into layers. Post-processing may include heat treatment and polishing of fabricated parts [10].
Selective Laser Sintering
An SLS printer uses a powder form of material for printing objects. A laser fuses a single layer of powder by drawing the shape of the object according to the first 2D cross-section of the 3D model. Immediately, the build platform is lowered by the defined layer thickness and another layer of powder is rolled across [10]. The process repeats, fusing each layer one at a time to form the object. SLS can be used with metal, ceramic, and plastic powders. The precision of the laser and the diameter of the powder determines the degree of detail of the final object, so it is possible to create detailed structures with an SLS printer [11].
 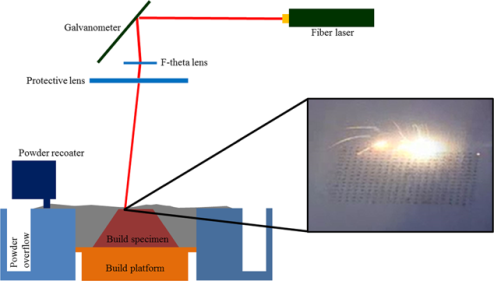
Figure 2: Schematic of SLS system. The key components of SLM include the laser system (a fiber laser, F-theta and galvanometer used to control the laser beam movement) and the mechanical system (movable build platform and powder roller) [10].
Electron Beam Melting
An EBM printer uses a powder form of material for printing objects, similar to SLS. However, while SLS uses a laser to fuse each layer of the powder, EBM uses an electron beam. This energy is delivered through an electric circuit between a tungsten filament inside of the electron gun and the build platform [10]. An electric current heats the filament to emit a beam of electrons [1]. Electric energy is transformed to heat energy which melts the powder on the build platform. The process continues similarly to SLS, where powder is spread across the platform in a thin layer, the cross-section of the object is melted, and then the build platform lowers by the layer thickness. A key element of EBM is that the build chamber is kept under vacuum, which allows the object to be maintain great detail (70-100μm) [1].
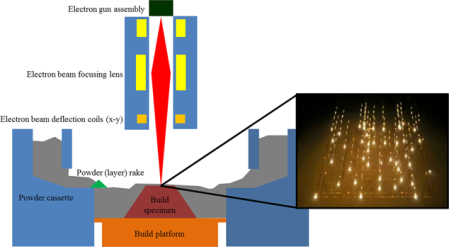
Figure 3: Schematic of EBM system. The key components of EBM include an electron beam system (electron gun assembly, electron beam focusing lens and deflection coils used to control the electron beam) and the mechanical system (movable powder rake and fixed powder cassettes) [10].
Materials of Medical Implants
The most common metals used for surgical implants are stainless steel 316L (ASTM F138), Cobalt based alloys (ASTM F75 and ASTM F799) and titanium alloy Ti-6Al-4V (ASTM F67 and F136) [12, 13]. However, these metals have disadvantages such as the potential release of toxic ions and particles due to corrosion that cause inflammation and allergic reactions, affecting biocompatibility [14]. Also, the materials that have an elastic modulus that is not similar to natural bone stimulate new bone growth poorly [12]. Despite this, the low Young’s modulus, high strength, and nonlinear elasticity of titanium-based alloys make it the least harmful choice [3]. The most commonly used titanium alloy is Ti-6Al-4V (Ti64) because it also has a better resistance to corrosion compared to stainless steels and cobalt-based alloys [15]. Additive manufacturing has also been done using Tantalum. Tantalum is biocompatible, hard, ductile, and chemically resistant, but it is expensive and difficult to machine [6]. Titanium based alloys are superior, thus Ti-6Al-V4 is the best material for additive manufacturing medical implants.
|
Material |
Young’s modulus (GPa) |
Ultimate tensile strength (MPa) |
Yield strength (MPa) |
Elongation (%) |
|
TiTa |
75.77 ± 4.04 |
924.64 ± 9.06 |
882.77 ± 19.60 |
11.72 ± 1.13 |
|
Ti6Al4V |
131.51 ± 16.40 |
1165.69 ± 107.25 |
1055.59 ± 63.63 |
6.10 ± 2.57 |
|
cpTi |
111.59 ± 2.65 |
703.05 ± 16.22 |
619.57 ± 20.25 |
5.19 ± 0.32 |
Table 1: Tensile properties of SLS produced TiTa, Ti6Al4V and commercially pure titanium samples (n = 5) [16].
Customized Implants
Additive manufacturing allows for the design and fabrication of customized prosthetic implants that are created to meet the specific needs of a patient, such as the size, shape, and mechanical properties of the implant. Additive Manufacturing reduces design time as well as manufacturing time because the implant pattern is computer generated with CT and MRI scans, thus removing the need for a physical model [8]. The ability to produce custom implants quickly solves a common problem with orthopedics where standard implants do not always fit the needs of certain patients. Previously, surgeons had to manually modify implants to make them fit the patient [7]. These techniques can be used by professionals in a variety of specialties such as neurosurgery, orthopedics, craniofacial and plastic surgery, oncology, and implant dentistry [8].
One example of an application in which a customized implant is required is craniofacial reconstruction. Craniofacial abnormalities are a diverse group of congenital defects that affect a large number of people and can be acquired at birth or due to injuries or tumors [8]. Standard cranial implants rarely fit a patient precisely because skulls have irregular shapes [7]. The custom implant can be created by using a CT scan to create a 3D virtual model of the patient’s skull. Then the model can be used with CAD software to design an implant that would perfectly fit the patient [8]. Using custom implants has shown to improve the morphology for large and complex-shaped cranial abnormalities, and some researchers have observed a greater improvement in neurological functions than after similar surgeries using traditionally manufactured implants [17, 18].
 
Figure 4: Skull model and customized implant for craniofacial reconstruction surgery [8].
Scaffold
Additive manufacturing medical implants allows the porosity of the surface to be designed, controlled, and interconnected, which provides better bone growth into implants, thus decreasing the chances of the body rejecting the implant. Additionally, the rough surface quality of 3D printed implants enhances bone-implant fixation [1]. Without scaffold, there is a risk of bone weakening and bone loss around the implant, which is a consequence of stress shielding due to high stiffness of materials [19]. The probability of this problem occurring is lessened when bone can grow into a porous surface of the implant [19].
Cellular lattice structures are classified by stochastic and non-stochastic geometries. The pores in stochastic structures have random variations in size and shape, while the pores in non-stochastic structures have repeating patterns of particular shapes and sizes [10]. The main challenge in additively manufacturing scaffolds is the difficulty to remove the loose powder from within the pores, but an advantage is that additive manufacturing technology allows for the manufacturing of different types of scaffolds if a design requires it; different regions of the implant could have different porosities [1, 10].
The procedure used to achieve the porous areas with traditional manufacturing methods includes coating a smooth surface with other materials such as plasma-sprayed titanium or a titanium wire mesh; however, combining different metals increases the risk of the body rejecting the implant. Additive manufacturing allows the smooth and porous surfaces to be fabricated with the same material, thus decreasing that risk. A variety of additive manufacturing techniques can be used to create the lattice structure, but scaffold can be fabricated by SLS or EBM without the need for support structures, thus making it the most effective method [5].
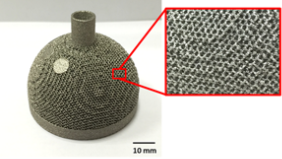
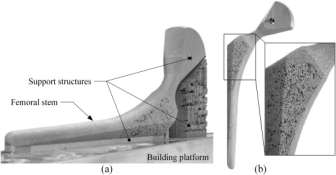
Figure 5: Acetabular cup with designedFigure 6: (a) Porous femoral stem on the building
porous surface [10].platform, (b) post-processed femoral stem [5].
Conclusion
There are many advantages to using additive manufacturing to fabricate surgical implants. These benefits include improved medical outcome, cost effectiveness, reduced surgery time, as well as customization and scaffold. Overall, the most effective type of additive manufacturing for the medical implant application is Electron Beam Melting because it can produce a high quality, high purity biocompatible implant that has the required mechanical properties. The recommended metal to use for most implants is the titanium-based alloy Ti-6Al-4V because of its low Young’s modulus, high strength, nonlinear elasticity, and corrosion resistance. Overall, additive manufacturing is an excellent production method for medical implants because it allows surgeons to customize implants and scaffold to the specific needs of the patient.
Â
References
1.Petrovic, V., et al., Additive manufacturing solutions for improved medical implants. 2012: INTECH Open Access Publisher.
2.Ahn, Y.K., et al., Mechanical and microstructural characteristics of commercial purity titanium implants fabricated by electron-beam additive manufacturing. Materials Letters, 2017. 187: p. 64-67.
3.Yan, L.M., et al., Improved mechanical properties of the new Ti-15Ta-xZr alloys fabricated by selective laser melting for biomedical application. Journal of Alloys and Compounds, 2016. 688: p. 156-162.
4.Caldarise, S., Hip joint prostheses and methods for manufacturing the same. 1996, Google Patents.
5.Simoneau, C., et al., Development of a porous metallic femoral stem: Design, manufacturing, simulation and mechanical testing. Materials & Design, 2017. 114: p. 546-556.
6.Wauthle, R., et al., Additively manufactured porous tantalum implants. Acta Biomaterialia, 2015. 14: p. 217-225.
7.Ventola, C.L., Medical Applications for 3D Printing: Current and Projected Uses. Pharmacy and Therapeutics, 2014. 39(10): p. 704-711.
8.Jardini, A.L., et al., Cranial reconstruction: 3D biomodel and custom-built implant created using additive manufacturing. Journal of Cranio-Maxillofacial Surgery, 2014. 42(8): p. 1877-1884.
9.D’Urso, P.S., et al., Custom cranioplasty using stereolithography and acrylic. British Journal of Plastic Surgery, 2000. 53(3): p. 200-204.
10.Sing, S.L., et al., Laser and electronâ€Âbeam powderâ€Âbed additive manufacturing of metallic implants: A review on processes, materials and designs. Journal of Orthopaedic Research, 2016. 34(3): p. 369-385.
11.Hoy, M.B., 3D printing: making things at the library. Med Ref Serv Q, 2013. 32(1): p. 94-9.
12.Kokubo, T., et al., Bioactive metals: preparation and properties. J Mater Sci Mater Med, 2004. 15(2): p. 99-107.
13.Staiger, M.P., et al., Magnesium and its alloys as orthopedic biomaterials: A review. Biomaterials, 2006. 27(9): p. 1728-1734.
14.Polo-Corrales, L., M. Latorre-Esteves, and J.E. Ramirez-Vick, Scaffold Design for Bone Regeneration. Journal of nanoscience and nanotechnology, 2014. 14(1): p. 15-56.
15.Dinda, G.P., L. Song, and J. Mazumder, Fabrication of Ti-6Al-4V Scaffolds by Direct Metal Deposition. Metallurgical and Materials Transactions a-Physical Metallurgy and Materials Science, 2008. 39A(12): p. 2914-2922.
16.Sing, S.L., W.Y. Yeong, and F.E. Wiria, Selective laser melting of titanium alloy with 50 wt% tantalum: Microstructure and mechanical properties. Journal of Alloys and Compounds, 2016. 660: p. 461-470.
17.Rotaru, H., et al., Cranioplasty With Custom-Made Implants: Analyzing the Cases of 10 Patients. Journal of Oral and Maxillofacial Surgery, 2012. 70(2): p. e169-e176.
18.Agner, C., M. Dujovny, and M. Gaviria, Neurocognitive Assessment Before and after Cranioplasty. Acta Neurochirurgica, 2002. 144(10): p. 1033-1040.
19.Shah, F.A., et al., Long-term osseointegration of 3D printed CoCr constructs with an interconnected open-pore architecture prepared by electron beam melting. Acta Biomaterialia, 2016. 36: p. 296-309.