Health Belief Model and Hypertension Treatment Compliance
Name of Journal: World Journal of Hypertension
ESPS Manuscript NO: 27556
Manuscript Type: BASIC STUDY
The health belief model and compliance with hypertension treatment
Running title: Health Belief Model and Compliance in Hypertension
Pauline E. Osamor and Olanike A. Ojelabi
Pauline E. Osamor,Institute of Child Health, College of Medicine, University of Ibadan, Nigeria,
Olanike A. Ojelabi,Worcester State University, Urban Studies Department, Worcester, MA 01605, USA
Author contributions: Osamor PE, contributed to the conception and design of the study; all authors contributed to the writing and critical revision of the manuscript.
Supported by: The data in this study is largely from the first author’s PhD thesis at the University of Ibadan, Nigeria, which was supported by African Doctoral Dissertation Research Fellowship (ADDRF).
Institutional review board statement: All consent forms, ethical permission and other participant information materials have been reviewed and given full approval by the Joint University of Ibadan/University College Hospital Health Research Ethics Committee.
Institutional animal care and use committee statement: This study does NOT involve the use of animal subjects.
Biostatistics statement: The study was designed, analysed and data interpreted by the authors. Data available in this manuscript did NOT involve a biostatistician.
Conflict-of-interest statement: The author reports no conflicts of interest in this work.
Data sharing statement: No additional data are available
Abstract
AIM: To explore the use of the Health Belief Model (HBM) in evaluating care seeking and treatment compliance among hypertensive adults in south-west, Nigeria.
METHODS: A community-based cross-sectional study was conducted using a semi-structured questionnaire to obtain information from 440 hypertensive adults in an urban, low-socio-economic community, situated in south west Nigeria. Focus Group Discussions (FGDs) were conducted with a subset of the population. The relationship between treatment compliance and responses to questions that captured various components of the HBM was investigated using chi-square tests. Content analysis was used to analyze data from the FGD sessions and to provide context to the survey responses. Data entry and management was carried out using the Statistical Package for Social Sciences (SPSS) version 11.0.
RESULTS: The components of the HBM reflecting Perceived Susceptibility components were significantly associated with treatment compliance. On the other hand, HBM Perceived Seriousness components were not significantly associated with compliance. The main HBM Perceived Benefit of Taking Action component that was prominent was the belief that hypertension could be cured by treatment, a theme that emerged from both the survey and the FGD.
CONCLUSION: Use of the HBM as a framework is helpful in identifying perceptions and behaviors associated with hypertension treatment compliance.
Key words: Health belief model; Compliance; Hypertension; Community-based; Nigeria
Core tip: Hypertension is a major health problem in developing and developed countries, and treatment compliance for such chronic conditions is often poor. In this study, the Health Belief Model (HBM) was used to evaluate care seeking and treatment compliance among hypertensive adults. HBM proved to be a valuable framework to develop and modify public health interventions and also serves to improve treatment compliance and reduce the risk of complications.
Osamor PE, Ojelabi OA. The health belief model and compliance with hypertension treatment. World J Hypertension 2017;
INTRODUCTION
Hypertension, otherwise known as high blood pressure, is a leading cause of cardiovascular disease (CVD) worldwide[1]. The proportion of the global burden of disease attributable to hypertension has significantly increased from about 4.5 percent (nearly 1 billion adults) in 2000 to 7 percent in 2010[2-9]. This makes hypertension a major global public health challenge and the single most important cause of morbidity and mortality globally. The prevalence of hypertension in Nigeria may form a substantial proportion of the total burden in Africa. This is because of the large population of the country currently estimated to be over 170 million[3,6,10]. In Nigeria, hypertension is the commonest non-communicable disease with over 4.3 million Nigerians above the age of 15 classified as being hypertensive using the erstwhile national guidelines (systolic BP > 160 mmHg and diastolic BP > 90 mmHg)[12-15].
Treatment of hypertension rests on a combination of lifestyle interventions and use of antihypertensive medication. However, poor compliance with treatment is often common in hypertension. Studies of treatment compliance have explored the role of various factors, including demographic and socio-behavioral features of patients, the type and source of therapeutic regimen, and the patient-provider relationship[16]. Yet, a common framework for evaluating such factors is often lacking. One such framework is the Health Belief Model (HBM),which has shown utility in evaluating compliance with antihypertensive medications[17-20].
Health Belief Model
The Health Belief Model (HBM) is an intrapersonal health behavior and psychological model. This model has been commonly applied to studying and promoting the uptake of health services and adoption of health behaviors[21]. Recently, a National Institutes of Health publication, “Theory at a Glance, A Guide for Health Promotion Practices” proposed that the HBM may be useful in the examination of inaction or noncompliance of persons with or at risk for heart disease and stroke[24], suggesting a natural fit for this study.
The HBM is a “value-expectancy” model [17]. It attempts to explain and predict health behaviors by focusing on the attitudes and belief patterns of individuals and groups. The modelconsists of six dimensions: perceived susceptibility, perceived severity, perceived benefits, perceived barriers, cues to action and modifying factors. While the HBM has been criticized for overemphasizing the logical order and rationality of one’s health behaviors[28], it is considered to be one of the most influential models in the history of health promotion practice[29], and has shown usefulness in predicting health behaviors among population with or at risk for developing cardiovascular disease.
With respect to care-seeking and treatment compliance, a hypertensive patient’s ability to see a physician and comply to medical treatment regimen is a function of a various factors. These include patient’s personal knowledge, benefit and perceptions, modifying factors, and cues to action[30]. Therefore, the goal of this study is to explore the use of the HBM as a framework for evaluating care-seeking and treatment compliance in hypertension in south-west Nigeria.
Rationale
Uncontrolled hypertension is caused by non-adherence to the antihypertensive medication, patients understanding their drug regimens and the necessity to adhere to this regimen will help to improve their adherence, thus help prevent the complications of hypertension that are debilitating and if not prevented can increase the burden of a disease that is already on the increase[31]. Knowledge and beliefs about hypertension have been frequently examined in efforts to better understand the disparities in blood pressure control[33,34]. Relatively few studies, however, have attempted to identify individual factors associated with the adoption of hypertension control behaviors using a health behavior model as the theoretical framework. Thus, this study aims to explore the use of the HBM- an intrapersonal health behavior and psychological model in evaluating care seeking and treatment compliance among hypertensive adults in south west Nigeria.
MATERIALS AND METHODS
This community-based cross-sectional study was carried out in an urban, low-socio-economic community in Nigeria. Most of the residents belong to the Yoruba ethnic group and the dominant religion is Islam. The health facilities in the community include an outreach clinic run by the Department of Preventive Medicine and Primary Care of the University of Ibadan, four private clinics and a small dental clinic. Other sources of health care in the community include Patent Medicine Vendors (PMVs) and three traditional healing homes. The study site was selected for three specific reasons: Firstly, the community has been the site of previous research studies where people were screened and therefore know of their hypertension status. Secondly, a community study approach (instead of a clinic-based approach) was chosen because selecting participants from a clinic or hospital will only select those who are attending clinic or complying, thereby introducing a selection bias and thirdly, the community has a variety of sources of healthcare located within the community, implying that residents have options when seeking healthcare.
The study is a community-based cross-sectional study which enrolled hypertensive adults (age 25 years and above) in the community. It utilized both the survey and Focus Group Discussion (FGD) to collect primary data from the respondents. The participants for this study were selected from a list of known hypertensive adults residing in the community that was developed from a previous hypertension study[35] and updated for the present study during home visits. Four hundred and forty (440) hypertensive subjects were enrolled using a consecutive sampling method.
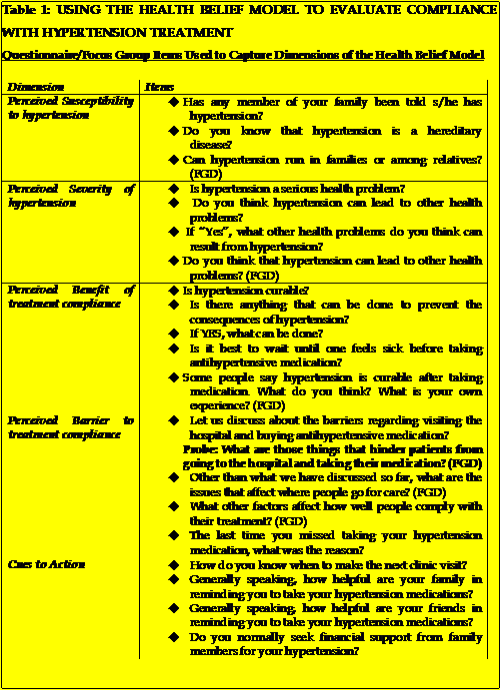
After obtaining informed consent, subjects were administered a semi-structured questionnaire that had items on several issues, including knowledge on causes, prevention and severity of hypertension, healthcare seeking for hypertension, their beliefs and perception about hypertension and compliance with treatment including keeping clinic follow-up appointments and regularly taking their antihypertensive medications. Eight FGDs were conducted, each with 6-8 discussants. The dimensions of the HBM were operationalized as described in table 1, where each dimension was framed as a series of questions, which were asked in the survey and/or discussed as a topic in the FGD.
Data entry and management was carried out using the Statistical
Package for Social Sciences (SPSS) version 11.0[36]. Univariate analyses were employed in interpreting socio-demographic characteristics of the respondents, while a bivariate analysis was used in cross tabulating variables. The transcription of the qualitative data was carried out immediately after each FGD session. This was essential since the memory of the interviewer/note taker was still fresh and it was easier to reconcile written notes and the interview transcripts. Content analysis was used to analyze data from FGD sessions.
RESULTS
Socio-demographic characteristics
A total of 440 (including 287 women) respondents were studied. The ages of respondents ranged from 25 to 90 years, with a mean of 60 (SD 12) years. Most (71%) of the respondents were married and 61.4%, Muslims. Slightly over half of the respondents (51.1%) had no formal education. About half (50%) of the respondents were traders, while those who have retired and not working constituted 25.7%.
Prevalence of compliance with clinic visits and taking medication
The prevalence of self-reported compliance with clinic appointments was 77.5% and that of good compliance with treatment was 50.7% of respondents. 41.5% reported poor treatment compliance at different levels ranging from regularly missing taking their medication to fairly regularly, sometimes and rarely taking their medication.
Perceived Susceptibility to hypertension
       In response to being asked what they understood by the disease “hypertension”, most respondents defined hypertension as an illness of anxiety and stress (60.9%). Nearly one in twelve (7.3%) said they did not know what hypertension meant. A few of the respondents (4.1%) believed that hypertension means “too much blood in the body”, thereby causing “tension in the blood”. Roughly two percent of respondents said hypertension “was in everybody’s blood”. A quote from one of the FGDs is illustrative:
Hypertension is in everybody’s body and blood. When we exert undue stress on our body, think too much and do a lot of wahala (stressful things), hypertension will start.
This statement clearly articulates the notion that everyone is predisposed to hypertension but the condition only becomes apparent or manifests itself when the person experiences a lot of stress. This could either mean that everyone is predisposed to having hypertension or that hypertension is hereditary.
Perceived Severity of hypertension
A large proportion 89.8% of the respondents knew that hypertension could lead to other serious health problems or complications. Only 1.1% did not affirm that it will lead to serious problem, while 9.1% did not know if hypertension could lead to other health problems. Other health problems that could result from hypertension mentioned by respondents include: stroke (47.5%); death (25.5%); severe headache (5.2%) and heart attack (5.0%). In the FGD sessions conducted, respondents were asked if they perceived hypertension to be a serious health problem. The general response was that hypertension is a serious health problem. One of the FGD discussants summed it this way:
Hypertension is a very serious sickness. It is not sickness we should take lightly. It can lead to quick death. One of my younger brothers who worked in the bank had hypertension. He suffered attacked from hypertension while in the office and before they got to the hospital, he died. Hypertension kills fast. But it has drugs that can control it and if one is not taking the drugs regularly, it will cause serious problem.
A fifty-two years old woman used her personal experience to buttress the magnitude of hypertension. She stated that:
This sickness they call hypertension is a very serious sickness. I was not taking any drugs because I did not have money to buy it and I was not worried because I was not feeling sick. In 2003, I was sick just for a week and before I knew what was happening I could not walk or move my body. I was rushed to the hospital and they told me my blood pressure was very high. I was in the hospital for almost a month and my children spent a lot of money. I am better now, but am still using walking stick because the hypertension made my body stiff. I am taking my medication always now so that I do not die quickly because it can kill.
The general perception of the respondents and focus group discussants on the complications from hypertension is that hypertension itself is a very serious health problem and that any complications arising from it could be very severe.
Perceived benefit of treatment compliance
Nearly three quarters (73.2%) of the respondents believed that hypertension could be cured with treatment. Most (72.0%) of the respondents reported that it is not good to wait until one feels sick before taking antihypertensive medication and the reason given by a large proportion (30%) of these respondents is that taking medication regularly will prevent reoccurrence of hypertension. Despite the fact that respondents believe they needed to take medication as prescribed (and not only when they are sick), only a relatively small proportion (a little above 50%) of the respondents did take their medication as prescribed.
Perceived barriers to complying with treatment
Among the respondents, 41.5% had poor compliance at different levels ranging from regularly missing taking their medication to fairly regularly, sometimes and rarely taking their medication. Of these respondents who were non-compliant with their medication, 11.4% said they felt better and therefore had no need to continue taking their medication. Only 0.5% said they were tired of taking drugs, while 6.8% stopped because of lack of funds to purchase drugs. Other factors included side effects of drugs (6.1%), forgetfulness (8.4%), busy schedule and limited medication (3.6%). A major theme from the survey and FGDs is that respondents were apprehensive of the long term effects from antihypertensive medication and the possibility of being stuck with it for the rest of one’s life or the medication causing other illness or complications. Negative feelings were elicited in some cases, as antihypertensive drugs were perceived as being damaging or “not good” for the body. The FGDs highlighted factors that hindered good compliance to treatment despite the general acceptance of the necessity to take antihypertensive medications. One of the discussant said:
I do not take my medicine every day. People do not always follow what doctor say. It is not only for hypertension, even for other sickness. If they say take medicine for five days, once we feel better by thethird day, the person will stop. Even the doctors themselves, will they swallow medicine every day?
A discussant in another session stated:
Let me tell you the truth … it is not easy to be taking drugs every day. Sometimes, we forget especially when you are rushing to go out. Sometimes we do not have the money to buy it.
Another respondent added details about what often happens as a result of the financial obstacles:
That is what we have all been trying to say. Money is the major problem. In the hospital, they will ask you to pay for ordinary card, before you see the doctor. When they write drugs for you there is no money to buy all. If you do not have money and you go to a private hospital, they will not even attend to you. That is why some people prefer to just go to chemist and buy what they can afford and some others prefer traditional medicine because you do not have to drink it every day and it is less expensive.
Cues to action
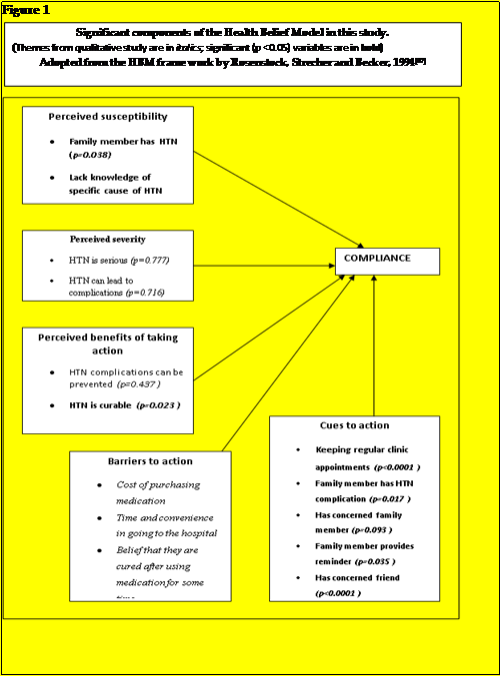
An important source of cues to action includes the individual’s cultural conditioning of available treatment options. In this study family and friends were a major source of cues to action. Overall, 19.3% of respondents reported that family members were very concerned about their hypertension while 74.8% said family members were extremely concerned about their hypertension. Also, 20.2% and 73.2% respectively reported that family members were very helpful or extremely helpful in reminding them about taking their medication. Regarding support from friends, 26.4% of respondents reported that friends were very concerned about their hypertension while 28.9% said friends were extremely concerned about their hypertension. Out of the 440 respondents, 91 and 150 (20.7% and 34.1%) respectively reported that friends were very helpful or extremely helpful in reminding them about taking their medication (Figure 1).
DISCUSSION
Hypertension is a condition of sustained high blood pressure which can only be confirmed after blood pressure measurements that meet the criteria for the condition. The cause of hypertension is not known in most cases[1] hence the term “essential hypertension”. In the present study, hypertension is perceived primarily as an illness of anxiety and stress. This finding is consistent with a previous study of hypertension in Nigeria[38] which revealed that over 60% of their respondents irrespective of the educational background believe that psychosocial stress is the main cause of hypertension. Similarly, Koslowsky et al[39] found that stress and tension were most commonly stated as causes of hypertension. Majority (more 90%) in this study believe hypertension is a serious condition and two-thirds (66%) believe that hypertension can be prevented. Contrary to findings and reports from previous studies[38,40,41], nearly three-quarters (73%) of respondents in the present study believe that hypertension is curable. Almost half of the respondents claim good compliance with respect to drug treatment and 86% claim good compliance with keeping their doctor’s appointment. Reasons for compliance to treatment include fear of the complications of hypertension and the desire to control blood pressure. Benson and Britten[42] reported that patients comply with medication regimen for a variety of reasons including perceived benefits of medication; fear of complications associated with hypertension and feeling better on medication. The latter reason is contrary to the generally held belief among physicians that hypertension is a largely asymptomatic disease[43].
One central theme that runs through the data in this study is the issue of socio-economic status of the respondents. This suggests the importance of considering other variables that can help form individual’s perception including health care costs and some sort of lay consultation that takes place before they resolve to take a recommended health action[27]. Financial hardship is a barrier which should not be ignored as it is a contributory factor to noncompliance. This finding corroborates the observed association between poor compliance, ignorance and lack of funds for purchase of drugs[44]. Failure of patients to keep scheduled appointments is an important obstacle to the provision of effective healthcare. By missing appointments, individuals deprive themselves of professional services. Interestingly, 77.5% of the respondents in this study claim they comply with keeping their follow up clinic appointments every time. Several studies have investigated HBM and appointment-keeping for chronic disease management. Nelson et al[20] and also Landers et al[45] found HBM variables to be unrelated to keeping clinic appointments for hypertension.
Social support networks are important in the long-term management of chronic conditions such as hypertension, which require a radical and life-long change in the lifestyle of the affected person. In this study, those who had support from friends or family members (concerned about their illness, giving reminders about medication) showed better treatment compliance than those who did not, although this difference was greatest for those that had the support of friends. This is an important finding and is consistent with what has been reported for multiple chronic diseases in several parts of the world[46].
 A summary of the major findings in this study in the context of interpreting compliance using the significant components of the HBM shown in Figure 1 suggests that HBM Perceived Susceptibility components tested were significant predictors of compliance. On the other hand, HBM Perceived Seriousness components were not significantly associated with compliance. The main HBM Perceived Benefit of Taking Action component that was prominent in this study is the belief that hypertension can be cured. This is a recurring theme in all the components of the study (survey and FGD) and most respondents believed that taking the medication for some time led to a “cure” and one could stop taking medication. This finding agrees with studies of Kamran et al[47], which showed a relationship between HBM constructs and treatment compliance. The constructs that were significantly showing relationship in their study were perceived susceptibility, perceived benefit of using the medicine and perceived barrier to treatment. This has major personal and public health implications because hypertension can only be controlled (not cured) and stopping medication can lead to complications. More importantly, it highlights the discrepancy between healthcare providers and their patients in the perceived goal of treatment since the former are working towards control while the latter believe compliance can lead to cure.
Most of the HBM Barriers to Taking Action components emerged during the FGD sessions. These barriers are practical issues that loom large and prevent the patients from making optimum use of the hospitals and medications that are available. In other words, the option of a university teaching hospital is available but is not accessible because of costs and inconvenience. Similarly, known medications that work well in hypertension are available but the costs are too high for the patients to comply with the prescriptions as written. It is noteworthy that believing that one can stop taking the medication after some time can also serve as a barrier to compliance because the individual now believes there is “no need” for more medication.
Another major finding from this study is that HBM Cues to Action are extremely important in predicting compliance with hypertension treatment in this community. These cues are centered on patients having family members and/or friends who are concerned about the individual’s health and treatment. This finding is important because, as noted by Harrison et al[48] in a meta-analysis, cues are often not included in Health Belief Model studies. Indeed, these authors limited their review to articles to the four major components of the HBM (susceptibility, severity, benefits and costs) because in their words: “Cues to action have received so little attention in empirical studies that we excluded this dimension”. However, the findings of this study shows that cues are an important dimension in these types of study. While the specific cues that are important may vary between locations, cultures, and environments, they emphasize the social context in which health behavior takes place. As expected, attending clinic regularly is an important predictor of compliance in the present study. It provides an opportunity for multiple cues that can improve compliance, including blood pressure checks, discussing actions to control blood pressure, and reminders to take medication.
CONCLUSION
Components of the HBM show variation in association with treatment compliance for hypertension in this Nigerian community. The findings provide useful baseline data for future studies of the Health Belief Model in hypertension and other chronic conditions in similar societies.
Strength and limitations of the study
Strengths of this study include: the use of both survey and FGD methods; inclusion of a large set of variables and focus on the components of the HBM to a non-communicable disease (hypertension) in a developing country context. A potential limitation is that the study did not formally investigate the modifying factors dimension of the HBM. Nonetheless, the findings provide clues to care-seeking and compliance issues, while suggesting potential intervention points (e.g. breaking the cost barrier, including social networks in treatment plans) that could be further studied and tested.
Ethical Approval
Ethical approval for the study was obtained from the Joint University of Ibadan /University College Hospital Ethical Committee.
Acknowledgment
The authors are grateful to the study participants and community leaders of Idikan community, Ibadan. The input of Dr. Bernard Owumi and Dr. Patricia Awa Taiwo of the Department of Sociology, University of Ibadan, is hereby acknowledged.
REFERENCES
1Mukhopadhyay, B. Detecting and preventing hypertension in remote areas. Ind. J Med Ethics 2006; 3(4): 124-5
2 Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the global burden of disease study 2010. The Lancet. 2012; 380(9859): 2224-60 [DOI: 10.1016/S0140-6736(12)61766-8]
3 Adeloye D, Basquill C, Aderemi AV, Thompson JY, Obi FA. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. J Hypertens 2015; 33: 230-242 [PMID: 25380154 DOI: 10.1097/HJH.0000000000000413]
4 Beaglehole R, Bonita R, Alleyne G, Horton R, Li L, Lincoln P, et al. UN high-level meeting on non-communicable diseases: addressing four questions. The Lancet 2011; 378: 449-455 [PMID: 21665266 DOI: 10.1016/S0140-6736(11)60879-9]
5 Alwan A, Armstrong T, Bettcher D, Branca F, Chisholm D, et al. Global status report on non-communicable diseases 2010. WHO 2011: Available online: http://www.who.int/nmh/publications/ncd_report_full_en.pdf
6 Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. The Lancet 2012; 380(9859):2095-128[DOI: 10.1016/S0140-6736(12)61728-0]
7 Whitworth JA. 2003 World Health Organization (WHO)/ International Society of Hypertension (ISH) statement on management of hypertension. J. Hypertens 2003; 21(11):Â 1983-92 [PMID: 14597836]
8 Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. The Seventh Report of the Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure: the JNC 7 report. JAMA 2003; 289(19): 2560-72 [PMID: 12748199]
9 Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. The Lancet 2005; 365(9455): 217-23 [PMID: 15652604]
10 WHO Regional Committee for Africa. Cardiovascular diseases in the African region: current situation and perspectives-report of the regional director 2005. Maputo, Mozambique: The WHO Regional Office for Africa (AFR/RC55/12). Available online: http://www.afro.who.int/en/fifty-fifth-session.html
11 Mocumbi AO. Lack of focus on cardiovascular disease in sub-Saharan Africa. Cardiovascular Diagnosis and Therapy 2012; 2(1): 74-7 [PMID: 24282699 DOI: 10.3978/j.issn.2223-3652.2012.01.03]
12 Kadiri S. Management of hypertension with special emphasis on Nigeria. Arch Ibadan Med 1999; 1: 19-21
13 Akinkugbe OO. Current epidemiology of hypertension in Nigeria. Arch. Ibadan Med 2003; 1: 3-5
14 Iyalomhe GBS, Omogbai EKI, Ozolua RI. Electrolyte profiles in Nigerian patients with essential hypertension. Afric. J. Biotech 2008; 7(10): 1404-1408
15 Ike SO. Prevalence of hypertension and its complications among medical admissions at the University of Nigeria Teaching Hospital, Enugu, Nigeria (Study 2). Niger J Med 2009; 18(1): 68-72 [PMID: 19485152]
16 Haynes RB, Taylor DW, Sackett DL, (1979). Compliance in health care. Johns Hopkins University Press: Baltimore, MD.
17 Becker MH, Maimon LA. Sociobehavioral determinants of compliance with health and medical care recommendations. Med. Care 1975; 13(1): 10-24 [PMID: 1089182]
18 Rosenstock IM. (1990). The health belief model: explaining health behavior through expectancies. In Glanz K, Lewis FM, Rimer BK (Eds). Health behavior and health education theory, research and practice (pp. 39-62). San Francisco, Jossey
19 Kirscht JP, Rosenstock IM. Patient adherence to antihypertensive medical regimens. J Community Health 1977; 3(2): 115-124 [PMID: 617631]
20 Nelson EC, Stason WB, Neutra RR, Solomon HS, McArdle PJ. Impact of patient perception on compliance with treatment for hypertension. Med Care 1978; 16(11): 893-906 [PMID: 713625]
21 Rosenstock I, Strecher V, Becker M. Social learning theory and the health belief model. Health Education Behavior 1988; 15(2): 175-183 [PMID: 3378902]
22 Glanz K, Rimer B, Lewis F. (Eds.) (2002). Health behavior and health education: theory, research, and practice (3rd ed.). San Francisco, CA: Jossey-Bass
23 Becker M. The health belief model and personal health behavior. Health Education Monographs 1974; 2(4): 324-353
24 U.S. Department of Health and Human Services, National Institute of Health, National Cancer Institute. Theory at a glance: a guide for health promotion practice. (2005). NIH publication no. 05-3896.
25 Wallston BD, Wallston KA. Locus of control and health: a review of the literature. Health Education Monographs 1978; 6(2): 107-117 [PMID: 357347]
26 Rosenstock IM. The health belief model and preventive health behavior. Health Education Behavior 1974; 2: 354-386 [DOI: 10.1177/109019817400200405]
27 Furnham A. Explaining health and illness: lay perceptions on current and future health, the causes of illness and the nature of recovery. Social Science and Medicine 1994; 39(5): 715-725 [PMID: 7973869]
28 Gillam S. Understanding the uptake of cervical cancer screening: the Contribution of the Health Belief Model. British Journal of General Practice 1991; 41(353): 510-513 [PMC 1371864]
29 Roden J. Revisiting the Health Belief Model: nurses applying it to young families and their health promotion needs. Nursing and Health Science 2004; 6(1): 1-10 [PMID: 14764188]
30 Owumi BE. (1996). Society and health: social pattern of illness and medical care. In E.A Oke & B.E. Owumi (Eds.), Readings in medical sociology (2nd ed.). Adjacent Press: Ibadan.
31 Kumar PN, Halesh LH. Antihypertensive treatment: a study on correlates of non-adherence in a tertiary care facility. Int J Biol Med Res 2010; 1: 248-52
32 Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003; 42(6): 1206-52 [PMID: 14656957]
33 Kressin N, Wang F, Long J, Bokhour BG, Orner MB, et al. Hypertensive patients’ race, health beliefs, process of care, and medication adherence. J Gen Intern Med 2007; 22(6): 768-774 [PMC 2219848 DOI: 10.1007/s11606-007- 0165-9]
34 Wyatt SB, Akylbekova E, Wofford M, Coady S, Walker E, Andrew M, Jones D. Prevalence, awareness, treatment and control of hypertension in the Jackson Heart Study. Hypertension 2008; 51(3): 650-656 [PMID: 18268140 DOI:10.1161/hypertensionaha.107.100081]
35 Osamor PE, Owumi .E. Complementary and alternative medicine in the management of hypertension in an urban Nigerian community. BMC Complementary and Alternative Medicine 2010; 10: 36 [PMC 2912779 DOI: 10.1186/1472-6882-10-36]
36 SPPS for Windows (version 11). Chicago: SPSS Inc; 1999.
37 Rosenstock IM, Strecher VJ, Becker MH. (1994). The health belief model and HIV risk behavior change. In DiClemente RJ, Peterson JL (Eds). Preventing AIDS: theories and methids of behavioral interventions (pp. 5-24). New York, Springer US.
38 Oke DA, Bamidele EO. Misconceptions of hypertension. Journal of the National Medical Assoc 2004; 96(9): 1221-1224 [PMC 2568468]
39 Koslowsky M, Croog SH, La Voie L. Perception of the etiology of illness: causal attributions in a heart population. Percept Mot Skills 1978; 47(2): 475-85 [PMID: 724385]
40 Spence JD, Hurley TC. Actual practice in hypertension: implications for persistence with and effectiveness of therapy. Current Hypertension Reports 2001; 3(6): 481-487 [PMID: 11734093]
41 Wizner B, Grodzicki B, Gasowski J. Knowledge about hypertension and blood pressure level. Przegl Lek 2000; 57(7-8): 402-405 [PMID: 11109314]
42 Benson J, Britten N. Patients’ decisions about whether or not to take antihypertensive drugs: qualitative study, BMJ 2000; 325(7369): 873 – 877 [PMID: 12386041]
43 Svensson S, Kjellgren KI, Ahlner J, Säljö R. Reasons for adherence with antihypertensive medication. Int J Cardiol 2000; 76(2-3): 157-163 [PMID: 11104870]
44 Isezuo AS, Opera TC. Hypertension awareness among Nigerians in a Nigerian tertiary health institution. Sahel Medical Journal 2000; 3(2): 93-9745 Landers R, Riccobene A, Beyreuther M, Neusy AJ. Predictors of long-term compliance in attending a worksite hypertension programme. J Hum Hypertens 1993; 7(6): 577-579 [PMID: 8114052]
46 Oxman TE, Hull JG. Social support and treatment response in older depressed primary care patients. J Gerontol B Psychol Sci Soc Sci 2001; 56(1): 35-45 [PMID: 11192336]
47 Kamran A, Sadeghieh AS, Biria M, Malepour A, Heydari H. Determinants of patient’s adherence to hypertension medications: application of health belief model among rural patients. Ann Med Health Sci Res 2014; 4(6): 922-927 [PMID: 25506487 DOI: 10.4103/2141-9248.144914]
48 Harrison JA, Mullen PD, Green LW. A meta-analysis of studies of the health belief model with adults. Health Educ Res 1992; 7(1): 107-116 [PMID: 10148735]