Nature of Cortical Bone
Â
- Nature of cortical bone from the millimeter to Nano-meter scale:
Likewise, with every organic tissue, cortical bone has a various leveled structure. This implies cortical bone contains a wide range of structures that exist on many levels of scale. The various leveled association of cortical bone is characterized in the table below:
Cortical bone structural organization:
|
Level |
Cortical structure |
Size range |
h |
|
0 |
Solid material |
>3000mm |
– |
|
1 |
Secondary Osteons (A) Primary Osteons (B) Plexiform (C) Interstitial Bone |
100 to 300mm |
<0.1 |
|
2 |
Lamellae(A,B*,C*) Lacunae(A,B,C,D) Cement lines(A) |
3 to 20mm |
<0.1 |
|
3 |
Collagen-Composite(A,B,C,D) |
0.06 to 0.6mm |
<0.1 |
Table 1 Cortical bone structural organization along with approximate physical scales.
A – Structures found in secondary cortical bone
B – Structures found in primary lamellar cortical bone
C – Structures found in plexiform bone
D – Structures found in woven bone
* – Structures present in B and C but much less than in A
Â
Figure 1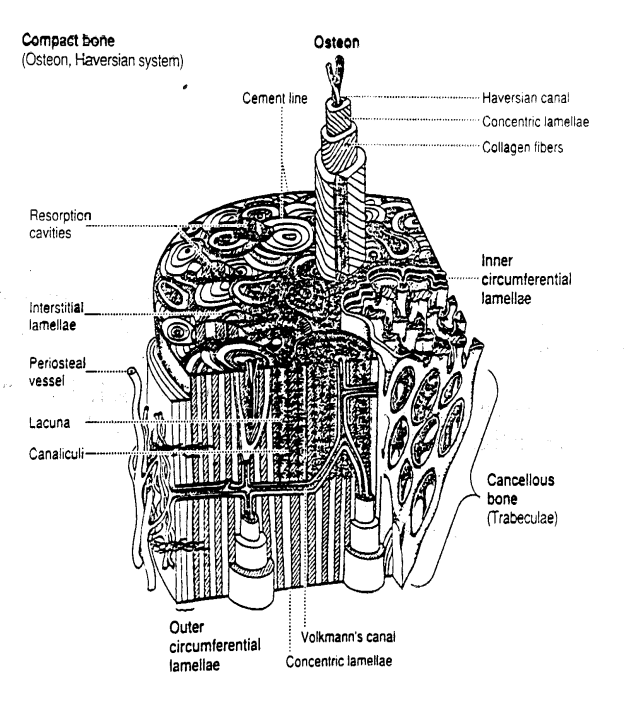
Cortical Bone’s Section view
Woven-fibered cortical bone:
Woven bone tissue is frequently found in extremely youthful developing skeletons less than 5 years old. Woven bone is accepted to be less thick in light of the free and muddled pressing of the sort I collagen filaments. woven bone is less hardened than different sorts of bone tissue in light of the commence that break callus is made predominantly out of woven bone and is a great deal less solid than typical bone tissue. Coordinate estimations of woven bone tissue solidness have not been made.

Plexiform Cortical Bone Tissue:
Figure 2 Plexiform Bone Section view
Plexiform bone emerges from mineral buds which develop first opposite and after that parallel to the external bone surface. This developing example creates the block like structure normal for plexiform bone. Every “block” in plexiform bone is around 125 microns (mm) crosswise over. Plexiform bone, like essential and optional bone, must be shaped on existing bone or ligament surfaces and can’t be framed all over again like woven bone. Because of its association, plexiform bone offers a great deal more surface territory contrasted with essential or auxiliary bone whereupon bone can be shaped. This expands the measure of bone which can be shaped in each time allotment and gave an approach to all the more quickly increment bone firmness and quality in a brief timeframe. While plexiform may have more noteworthy firmness than essential or optional cortical bone, it might do not have the break capturing properties which would make it more appropriate for more dynamic species like canines (pooches) and human
Â
Primary Osteonal Cortical Bone Tissue:
they don’t contain the same number of lamellae as auxiliary osteons. Likewise, the vascular channels inside primary osteons have a tendency to be smaller than optional osteons. Consequently, primary Osteonal cortical bone might be mechanically more stronger than secondary Osteonal cortical bone
Secondary Osteonal Cortical Bone Tissue:
Auxiliary osteons contrast from essential osteons in that optional osteons are framed by substitution of existing bone. Auxiliary bone outcomes from a procedure known as remodeling. In rebuilding, bone cells known as osteoclasts first resorb or destroy an area of bone in a passage called a cutting cone. Taking after the osteoclasts are bone cells known as osteoblasts which then frame issue that remains to be worked out up the passage. The osteoblasts top off the passage in stunned sums making lamellae which exist at the second level of structure. The osteoblasts don’t totally fill the cutting cone however leave an inside part open. This focal bit is known as a Haversian channel (see cortical bone schematic). The aggregate breadth of an auxiliary osteon ranges from 200 to 300 microns (meant as mm; equivalent to 0.2 to 0.3 millimeters). Notwithstanding osteons, optional cortical bone tissue likewise contains interstitial bone (umich.edu, n.d.)
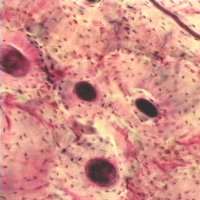
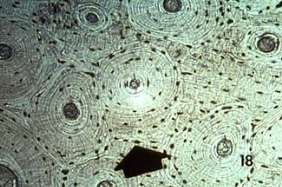

Figure 3 Secondary Osteonal Cortical Bone Tissue
Â
Performance of Bone as a tough and light material:
Most long bones appear, at first sight, to be unduly firm for the capacity they need to serve. If distinctive ones are made of bone material with similar properties, the thicker they are, the stiffer they will be. They will likewise, obviously, be heavier. Consequently, it may appear that there is a basic tradeoff amongst solidness and mass. Notwithstanding, one can’t consider the firmness and mass of the bone alone. One must consider additionally the mass of the muscle and bone framework together. Regularly, as when a weight is held in the hand with the elbow twisted, the framework ought not divert at all affected by a heap. Assume that the muscle is equipped for bearing the heap. To do this, it needs a specific cross-sectional area, however its length is irrelevant.
The load is appied through the hand toward the end of the bone, which will avoid to some degree, however the diversion can be taken up by compression of the muscle. On the off chance that the bone were thin and in this way light, yet adaptable, then after the load was applied, the muscle would need to get far to balance the extensive diversion of the finish of the adaptable bone. Assuming, on the other hand, the bone was stout and along these lines heavy, however stiff, after a similar load was applied, the muscle would need to contract just a short approach to balance the slight adaptability of the bone. The muscle appended to the adaptable bone would need to be longer, in light of the fact that there is more redirection in the unresolved issue up, than the muscle joined to the solid bone, and on the grounds that the two muscles must have same cross-sectional zone, the muscle connected to the more adaptable bone would accordingly be heavier.
As it were, one is paying for daintiness in the bone by weight in the muscles and the other way around. The pinnacle worries in the bone would be around 75 MPa when the framework was lightest. What is fascinating about this outcome is that the anxiety esteem is generally the same as the most extreme burdens found in the legs of numerous warm blooded animals amid strenuous exercises, for example, running quick or bouncing. At the end of the day, if bones were intended to have an adaptability that would limit the mass of the bone-muscle framework, the anxieties forced by the muscles would be of the request of 75 MPa, and this is generally what we find that bones are uncovered to. It might be, in this way, that the security considers that we see bones are, inexactly, controlled by the ideal firmness for least general weight. In the event that bone material were considerably weaker than it really is, bones would be heavier, thus drive the relationship, and they would be stiffer than was ideal for least mass.
Â
Remodeling of Cortical Bone and Cancellous Bone:
- Cortical bone:
- remodels by osteoclastic tunneling (cutting cone)
- osteoclastic resorption > layering of osteoblasts > layering of lamellae > cement line laid down.
- osteoclast make up head of cutting cone, followed by capillaries and then osteoblasts which lay down the osteoid to fill the cutting cone.
- sclerostin inhibits osteoblastogenenesis to decrease bone formation.
- cortical bone continues to change over time.
- cortical area decreases as age increases
- linked to increase fracture risk
- medullary canal volume increases as age increases
- cortical area decreases as age increases
- Cancellous bone remodels by
- osteoclastic resorption
-
osteoblastic deposition of layers of lamellae (Moore, n.d.)
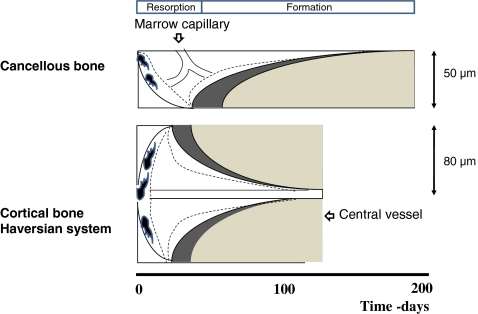
Figure 4 Bone rebuilding cavity diagram. (Disord, n.d.)
Bone remodeling happens in what Frost named the Basic Multicellular Unit (BMU), which includes the osteoclasts, osteoblasts, and osteocytes inside the bone-rebuilding cavity (Fig. 4). In cancellous bone rebuilding happens on the surface of trabeculae and keeps going around 200 days in ordinary bone. The rebuilding cycle can be as short as 100 days in thyrotoxicosis and essential hyperparathyroidism and surpass 1,000 days in low turnover states like Myxedema and after bisphosphonate treatment. Remodeling is started by osteoclastic resorption, which dissolves a resorption lacuna, the profundity of which fluctuates between 60 in youthful people and 40 μm in more established people. The resorption time frame has a middle span of 30-40 days and is trailed by bone development over a time of 150 days (Fig. 4). In typical bone the aftereffect of the remodeling cycle is finished refilling of the resorption lacuna with new bone. In sickness states like osteoporosis, the fundamental deformity is that the osteoblast can’t refill the resorption lacuna prompting to a net loss of bone with each remodeling occasion. In cortical bone remodeling continues in passages with osteoclasts framing “cutting cones” evacuating harmed bone took after by refilling by osteoblasts in the “end cone” happening behind the osteoclasts. In typical bone the span of the renovating cycle in cortical is shorter than in cancellous bone with a middle of 120 days. The aggregate surface of cancellous bone is totally renovated over a time of 2 years. As opposed to renovating destinations in cancellous bone, which are near red marrow, known to contain osteoprogenitor cells, rebuilding locales in cortical bone are far off from red marrow. Thusly, it was expected that the components of bone remodeling were distinctive in cancellous versus cortical bone, i.e. that the cells required for bone rebuilding in cancellous bone voyaged straightforwardly from the red marrow to bone surfaces in cancellous bone, while cells achieved cortical remodeling destinations bone by means of the vasculature. (Eriksen, n.d.)
Targeted and non-targeted remodeling:
Through its steady removal and renewal of damaged bone, bone redesigning secures skeletal trustworthiness all through life. It has turned out to be standard to recognize targeted on and non-targeted on (stochastic) rebuilding. Non-targeted on rebuilding means control renovating by hormones like PTH, thyroxine, development hormone and estrogen, additionally antiresorptive medications like bisphosphonates may influence non-targeted on redesigning. It appears that the primary pathway is through regulation of osteoclasts, which then by means of the coupling amongst resorption and development along these lines influences osteoblast movement. Directed redesigning secures expulsion of harmed bone through targeted resorption. Osteocytes are the most plenteous cells in bone, and their passing by microdamage has been recommended to be the significant occasion driving in the start of osteoclastic bone resorption. In typical bone. Resorption lacunae are 3 times more regular in relationship with microcracks, showing that redesigning is related with repair of such microdamage. Harmed osteocytes advance separation of osteoclast forerunners driven by discharge of M-CSF and RANKL. In cortical bone there is confirmation to recommend, that microdamage enacts new BMUs, as well as may direct the development of existing BMUs as they passage through the cortex. It likewise appears that the level of harm to the osteocyte organize decides osteocyte metabolic reactions to stacking and impacts targeted on renovating.
Investigation of the relationship of between mean microcrack length and BMU resorption space thickness in cortical bone shows that BMUs have a powerful region around 40 times more prominent than their genuine cross-area, which proposes that osteoclasts in the cutting cone of cortical BMUs can detect and direct toward microdamage. The connection amongst microdamage and start of bone renovating is further validated by the way that osteoclastic resorption is expanded in old bone.
how cells are effected by mechanical loads, fluid or forces:
In physical movement, mechanical strengths are applied on the bones through ground response forces and by the contractile action of muscles. These physical strengths result in an upkeep or pick up of bone mass, additionally drive adjustment of bone structure. The adjustment of trabecular bone engineering as per the requests of mechanical utilization is apparent in the vertebrae, where the trabeculae are transcendently situated in the longitudinal course, giving the most ideal imperviousness to pressure break of the vertebrae with an insignificant utilization of material. A great case of the empowering impact of mechanical stimuli on bone mass is given by the bones in the lower arm of tennis players. The ulna and radius in the arm that holds the racket are presented to high effect forces, prompting to little distortions in the hardened bone grid and an expansion in bone mass of 5 to 10% contrasted with the ulna in the contra-parallel arm. The distortions that happen in bones subsequently of physical forces are communicated as strain, where 1,000 microstrain breaks even with a 0.01% change long of the bone contrasted with its unique length. Lively exercise prompts bone strains up to 1,000 microstrain in people. By examination, controlled episodes of entire bone stacking bringing about 1,000 to 3,000 microstrain are anabolic in exploratory creature models of one-stacking, exhibiting the potential for fitting physical exercise schedules as a way to improve bone mass.
The cells likely in charge of detecting the physical stimuli got from mechanical forces applied on bones are the osteocytes, which include more than 90% of the bone cells. Osteocytes are stellate cells that are inserted inside the calcified bone framework. They shape an extensive number of cell-cell contacts through their long slim cell forms, framing a syncytium fit for fast transduction of signs. Osteocytes are exceptionally mechanosensitive, likely more so than periosteal fibroblasts or osteoblasts, and change the creation of a large number of flagging particles when activated by a mechanical force. Mechanically initiated osteocytes create flagging atoms like bone morphogenetic proteins (BMPs), Wnts, prostaglandin E2 (PGE2), and NO, which can adjust the enrollment, separation, and action of osteoblasts and osteoclasts. Along these lines, osteocytes are hypothetically equipped for coordinating bone adjustment in light of mechanical stimuli. The loss of bone mass after rear appendage emptying of mice was forestalled when 80% of the osteocytes were removed. Osteocytes accordingly appear to empower osteoclast action without day by day mechanical burdens, a capability that has been affirmed in vitro thinks about. To be sure it has been indicated as of late by two free gatherings that RANKL generation by osteocytes decides bone mass in grown-up mice, showing the significance of osteocytes in the control of bone mass. Strangely, a similar review exhibiting the prerequisite of osteocytes for intervening emptying instigated bone misfortune likewise demonstrated that the anabolic reaction of unresolved issue (does not require the nearness of living osteocytes. Be that as it may, this does not wipe out the part of osteocytes in intervening the anabolic reaction of unresolved issue under typical conditions.
If osteocytes are the expert mechanosensing cells of bone, then how do these cells sense entire bone burdens? One prominent hypothesis involves that network trains encompassing the osteocyte cell forms drive a thin layer of extracellular fluid encompassing the osteocyte cell procedures to stream over a weight angle. This stream of fluid “opens up” nearby strains, and is along these lines the mechanical signal that is eventually detected by the osteocytes. There is adequate exploratory proof to bolster disfigurements of the bone grid drive an interstitial fluid stream. A stream of additional cell fluid around the osteocytes thus of bone tissue strains, by stacking of sheep tibiae and taking after the dispersion of tracers through the lacuno-canalicular system. All the more as of late, Price et al.(2011) utilized fluorescence recuperation in the wake of photobleaching for imaging fluid dislodging synchronized with mechanical stacking, to demonstrate that the mechanical stacking of mouse tibia upgraded fluid transport through the lacuno-canalicular framework, exhibiting the connection of canalicular fluid stream with mechanical load. Moreover, a few agents announced that it is not the measure of strain connected to an entire bone that impacts bone development, yet the rate at which the strain is connected.
Disord, R. E. (n.d.). Rev Endocr Metab Disord. Retrieved from Reviews in Endocrine & Metabolic Disorders: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3028072/figure/Fig1/
Eriksen, E. F. (n.d.). Reviews in Endocrine & Metabolic Disorders. Retrieved from Reviews in Endocrine & Metabolic Disorders: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3028072/
Moore, D. (n.d.). Orthobullets. Retrieved from Orthobullets: www.orthobullets.com/basic-science/9008/bone-remodeling
umich.edu. (n.d.). Introduction to Biosolid Mechanics. Retrieved from umich.edu: http://www.umich.edu/~bme332/ch9bone/bme332bone.htm