Shared Care Plans: Risks and Opportunities
Introduction
Shared care in healthcare spans an extensive range of diseases, treatments and total care services across many medical disciplines. The predominant focus of this essay will be the patient in receipt of these vital shared care services. Patient care services and treatment plans should address all the needs presented by each patient’s unique medical situation. Unfortunately, the care needed for some paediatric patients with complex chronic comorbidities can just become far too complex to ever realistically be safely and effectively cared for in a homecare environment removed from their secondary care facility. This essay will highlight some common areas of difficulties and challenges which can lead to various errors across different ailments where shared care services are prevalent. On review of the literature two common areas of potential error that are obvious are as follows: –
- The communication of changes in a patient’s healthcare treatment (Coleman and Berenson, 2004): –
These communication messages (or ideally open access to a national online EHR) should incorporate all the multidisciplinary team which expands across a complex labyrinth of disciplines. Often these important messages (which provide a health information exchange, HIE) fail to get delivered to the relevant caregivers within the relevant time frame in order for the correct action to be taken (Rinner et al., 2016).
- Medication prescription errors: –
These are commonly the highest category of errors in the continuous care of patients in all care settings whether in secondary, primary or homecare.
This essay will also focus on the paediatric setting because of the importance for us to protect and strive to improve care to the most vulnerable. Attention has been given to information technology solutions, proposals and systems during the literature reviewing process.
Shared Care (Patient related reasons for homecare)
It has been proven that when you allow a child to leave their secondary care institution and return home to a homecare shared service that the risk of hospital borne infections are reduced and general quality of life and happiness are improved, this can result of shorter hospitalisation stays (Hudson et al., 2014).
The development of shared care in the field of Paediatric Oncology started in Ireland twenty-five years ago. These family-centred homecare services will often be a mix of ‘parent’ care with community care assistance, normally involving a team of medics, pharmacists, nurses, social workers, dieticians and other allied healthcare professionals. The HSE has published a final draft ‘New National Model of Care for Paediatric Healthcare in Ireland’ which hopefully will be adopted as it addresses most of the key areas relating to shared care at home (HSE, 2016). This HSE proposal will heavily rely on an expandable ICT service and the initiatives that are currently being evolved and developed within eHealth Ireland.
Shared care centres for paediatric cancer manage common side effects from the patient’s main treatment, they deliver supportive care to the patients and their main caregivers. During oncology treatments patients become vulnerable and fatigued, for these patients and their strained families/caregivers who would have had to travel long distances from home to their secondary care centre, can by continuously travelling, bring on a relapse in health to the patient. Home Treatment is the answer for these patients but home treatment can also bring on a set of new challenges for the patient’s main caregivers. On many occasions this can leave families and caregivers short on nursing care hours for their sick child. In Ireland, a few charitable organisations have been set up to help struggling families with sick children who want and need to be in their home environment. The Laura Lynn charity provides extra services for children and their families (when the national system in Ireland falls short) allowing them Respite, Crisis, Transitional and End of Life care assistance in many ways including nursing hours and a home from home (no care like home care) when required. https://lauralynn.ie/families/what-we-do/#.WMhiun9sZ_k.
Challenges and Opportunities
One of the biggest challenges with shared care plans is the length of time the patient is away from the tertiary centre that treats them for their condition, (either attending a local hospital/care centre or utilising a home care package from the community), is the potential for errors to occur during treatments. For example, medication errors have such a negative impact on patient outcomes and research shows these negative incidences can be reduced with the correct use of an ePrescribing decision support and drug delivery checking system (Meyer-Massetti et al., 2012).
In relation to homecare, the main caregiver is often required to perform as a Nurse, Pharmacist, Parent, Physiotherapist and Dietician and normally expected to administer intricate drugs without the support of a double-checking ‘manual’ or ‘electronic’ system available in a Hospital.
In a study of 117 paediatric oncology outpatients visits 18.8% were linked to a medication error in which 15 errors resulted in injury and 64 of the 117 errors were likely to cause harm. These errors regularly arose in the administration phase (56%)Â (Walsh et al., 2009). Walsh’s findings recommended that intervention targets including enhanced correspondence about prescription administration within the OPD clinic and home.
Lighthouse Projects Initiative
In 2016 the Irish health service (HSE) through eHealth Ireland has invested in three ‘lighthouse projects. These exciting projects are in the medical fields of Epilepsy, Haemophilia and Bipolar Disorder. Elements of this integrated health approach mirrors back to the potential errors in shared care that this essay has been identifying and will address the situations where the errors occur using ICT technology to improve communication and medication prescription monitoring, including many other benefits unique to each separate project, as stated about the bipolar disease project “This will use technology to enable self-management and the detection of early warning signs of relapse, thus empowering the patient” (eHealthIreland(2), 2016).
These projects are building an understanding and demonstrating the positive effects that a national connected EHR would bring the Irish healthcare system. Furthermore, using the proposed national individual health identifier (IHI) in these projects will aid cohesion moving forward to a full electronic patient record in primary and secondary healthcare.
Across the three projects communication and medication safety doesn’t stop at secondary or primary healthcare but this approach will empower the patient via a ‘patient portal’ and a mobile application. The diagram below shows the structure needed to ensure a full coverage of care.
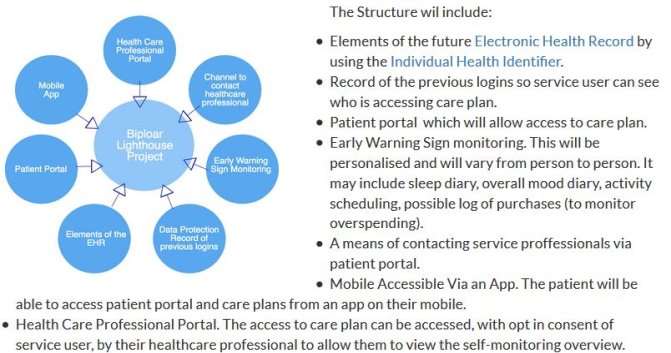
Fig 1:- http://www.ehealthireland.ie/images_upload/Library/Document-Library/Bipolar/Bipolar%20Lighthouse%20Proj%20Image.png
New Children’s Hospital (NCH) Spoke & Hub Solution
The New Children’s Hospital service model is a shared care approach to emergency care and satellite out-patient’s departments. The building site has now been cleared for this one billion euro Children’s Hospital on the St. James’s Hospital Campus.
What is interesting is the ‘Hub & Spoke’ solution (Fig 2) being used for these satellite centres; this is part of the new model of care for paediatric services in Ireland.

Fig 2: – http://www.newchildrenshospital.ie/clinical-vision/
The two Satellite Centres, one at Tallaght Hospital and the other at Connolly Hospital Blanchardstown will provide urgent care with better local access to trauma orthopaedics OPD services, home based and community services, diagnostics and chronic disease management, “where consultant-led emergency care will be delivered. These urgent care units will have observation beds and state-of-the-art diagnostic imaging and x-ray equipment” (NCHDB, 2015).
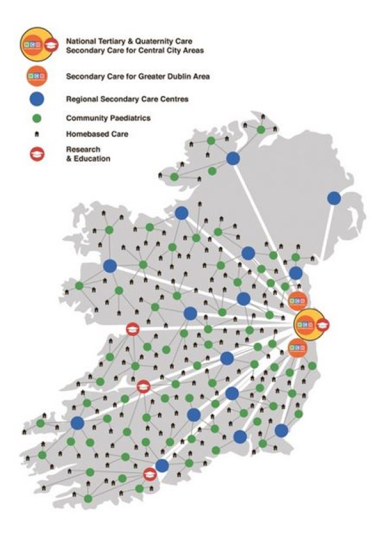
Fig 3: – http://www.newchildrenshospital.ie/clinical-vision/delivering-the-right-care-in-the-right-place-at-the-right-time-by-the-right-staff/
The HSE is Replacing the three old children’s hospitals with one mighty flagship plus two satellite centres (and a new model of care). The benefits of this new structure (due to space restrictions in a city centre site) might not be initially obvious but the fact that this will be a HIMSS Level 7 facility and because of the integration and sharing of knowledge across these sites will in theory benefit patient care and outcomes, “clinical-vision delivering the right care in the right place at the right time by the right staff” (NCHDB, 2015).
Conclusion
In order to have the desired optimal and fully functioning shared care network many changes will need to be forthcoming.
Predominantly, modifications with regards to care processes, the transmission and utilisation of information (to enhance better clinical decision making and communication) between clinicians in the shared care setting need to be achieved.
A shared model of care needs as it’s foundation stone a fully integrated ICT system and skilled personnel to operate it. Sound telecommunication links between shared care stakeholders locally, regionally and nationally will be key to the efficient and effective operation of shared care services.
In addition to effective communication it is essential that ICT links will support the current local and national clinical information systems (CIS) solutions that have been developed and deployed already (i.e. NIMIS) to support medical staff, healthcare professionals, pharmacists and key caregivers.
From the above it is clear that the Irish approach (and significant investment into eHealth Ireland) using ICT solutions in healthcare is taking positive strides in the desired direction in a field fraught with complexities.
Fortunately, within ten years, ‘the proof will be in the pudding’, so to speak, as we will be in the situation where we can look back and analyse the success (or failures) of the system that is now in development.