Suprascapular Neuropathy in Overhead Athletes
SUPRASCAPULAR NEUROPATHY IN OVERHEAD ATHLETES: A SYSTEMATIC REVIEW ON AETIOLOGY AND TREATMENT OPTIONS
Surya.P, Pankhania. R, Funk.L
ABSTRACT
Suprascapular neuropathy is often overlooked as a cause for shoulder pain in overhead athletes. However, with recent advancements in the understanding of the condition as well as its treatment methods, suprascapular neuropathy is now diagnosed more frequently. Consistent overhead activities, rotator cuff tear and direct compression of the nerve, by space occupying lesion are important etiologies for suprascapular neuropathy. While MRI is widely used to identify space-occupying lesions and rotator cuff injury; Electromyography (EMG) and Nerve Conduction Velocity (NCV) remains gold standards for confirming injury to the nerve. Conservative physical therapy, nerve blocks and arthroscopic and open surgical interventions are the main treatment plans for suprascapular neuropathy.
1. INTRODUCTION AND BACKGROUND
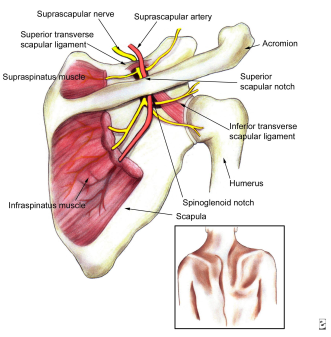 The posterosuperior aspect of shoulder receives its sensory innervation from the suprascapular nerve. The suprascapular nerve also provides motor innervation to supraspinatus and infraspinatus muscles. Compression or traction of nerve and rotator cuff diseases are found to be associated with suprascapular nerve damage and neuropathy. Clinical symptoms of the condition include pain in the posterior shoulder, feeble forward flexion, and weak external rotation. It is also noteworthy that the multiple presentations for suprascapular nerve neuropathy vary greatly in different patients and thus diagnosis of the condition is often challenging. This kind of nerve damage is a less common reason for shoulder pain and dysfunction in the general population, however is widely observed in athletes who play overhead sports such as volleyball, tennis, badminton, and baseball. Such sports expose the athlete’s hands to overhead, abducted and externally rotated positions for prolonged periods of time. (Cummins & Schneider, 2008).
The posterosuperior aspect of shoulder receives its sensory innervation from the suprascapular nerve. The suprascapular nerve also provides motor innervation to supraspinatus and infraspinatus muscles. Compression or traction of nerve and rotator cuff diseases are found to be associated with suprascapular nerve damage and neuropathy. Clinical symptoms of the condition include pain in the posterior shoulder, feeble forward flexion, and weak external rotation. It is also noteworthy that the multiple presentations for suprascapular nerve neuropathy vary greatly in different patients and thus diagnosis of the condition is often challenging. This kind of nerve damage is a less common reason for shoulder pain and dysfunction in the general population, however is widely observed in athletes who play overhead sports such as volleyball, tennis, badminton, and baseball. Such sports expose the athlete’s hands to overhead, abducted and externally rotated positions for prolonged periods of time. (Cummins & Schneider, 2008).
Observational studies have identified that players involved in overhead sports are at higher risk of injuries related to overuse of the shoulder such as rotator cuff tendinopathy and tearing of glenoid labrum (Pillai et al. 2011). On the other hand, shoulder pain due to suprascapular neuropathy is observed in only 1-2% of cases and therefore, the condition is often overlooked during diagnosis for shoulder pain (Boykin et al. 2010). Among the overhead sports athletes, incidences of suprascapular neuropathy are maximum in volleyball players. Around 33% of volleyball players suffer from this condition at some instance in their career (Boykin et al. 2010).
Traditionally, suprascapular neuropathy has always been regarded as a diagnosis of exclusion. However, now with further understanding of the etiology and advanced diagnostic options, the condition is being recognised by physicians from an earlier onset.
2. AETIOLOGY FOR SUPRASCAPULAR NEUROPATHY
Rotator cuff tear is considered as a prime cause for suprascapular neuropathy. Studies show that suprascapular neuropathy can also develop secondary to traction and microtrauma, especially in overhead athletes, particularly due to tightening of the spinoglenoid ligament during the overhead throwing position. The risk for the development of suprascapular neuropathy also increases in patients with ossification of the transverse scapular ligament or spinoglenoid ligament. Other causes such as; compression of the nerve at spinoglenoid notch due to the presence of a bone tumor, cyst due to labral, soft tissue or capsular injury tissue can also lead to the condition. Suprascapular neuropathy is also rarely seen following brachial neuritis, glenohumeral dislocation, fracture of the shoulder girdle, and penetrating or iatrogenic injury to the nerve (Lewis et al. 2012).
All these etiological factors for suprascapular neuropathy are discussed in detail in the following section.
2.1 Rotator Cuff Injury:
Anatomically, the suprascapular nerve branches from the upper trunk of the brachial plexus. From there, it travels posterior to the clavicle, passes below the transverse scapular ligament and then enters the suprascapular notch. The motor branches innervate the supraspinatus, and the nerve continues past the spinoglenoid notch and innervates the infraspinatus. Injury due to traction or compression of the nerve at any point in this path can lead to suprascapular neuropathy. Retracted superior or posterior rotator cuff tear is the most common cause for suprascapular nerve traction injury. Tension on the suprascapular nerve lying at a suprascapular notch or spinoglenoid notch increases with the retraction of supraspinatus and infraspinatus tendons. Studies on cadavers by Gosk et al (2007) showed that as the retraction of supraspinatus tendon increases, it reduces the angle between the suprascapular nerve and its first motor branch, which leads to an increase in tension and thus causes traction injury. Gosk et al. (2007) also found that massive rotator cuff tear was the main reason for suprascapular neuropathy in eight different overhead players. On the other hand, studies by Lajtai et al. (2009) found that rotator cuff tear and muscle atrophy were responsible for only 8% of suprascapular neuropathy cases.
Expanding the knowledge on the topic, different studies also showed that the tension between rotator cuff, supraspinatus and infraspinatus tendons has a profound impact on the condition of the suprascapular nerve. Observations of cadaver showed that the tension on the neurovascular pedicle increases significantly once the lateral advancement of a retracted rotator cuff tear exceeds 3 cm (Greiner et al. 2003). Other studies suggest that if the rotator cuff extension increases by 3 cm, it lay significant tension on the motor branches of the suprascapular nerve. Also, the tension on the medial portion of the suprascapular nerve starts to increase only by 1 cm extension of the rotator cuff. Increased tension is one of the important reasons for traction injury to the nerve (Larissa et al. 2014).
It has also been reported that following surgical repair of rotator cuff tear, the tendons can be advanced up to 3.5 cm without any significant risk to the health of suprascapular nerve. Various reports suggest that surgical repair of rotator cuff tear can help in either partially or completely resolving suprascapular neuropathy. Nerve recovery by reinnervation has been found in patients of suprascapular neuropathy following partial or complete arthroscopic rotator cuff repair (Petra et al. 2013).
2.2 Nerve injury: Sports Specific Etiology:
Sports physiotherapists have proposed various etiological mechanisms for suprascapular neuropathy which includes repeated traction, microtrauma, ischaemia of the nerve and compression of the nerve by soft tissue, tumor or cyst. However, the majority of the healthcare professionals consider that nerve injury due to repetitive trauma is the main reason for the development of suprascapular neuropathy.
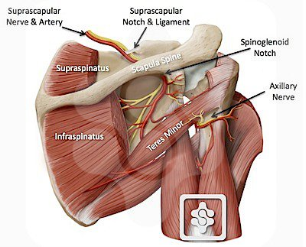 Two main sites for suprascapular nerve injury are: the suprascapular notch and the spinoglenoid notch. The symptoms alongside clinical presentation for suprascapular neuropathy thus depend on the location of nerve injury. Injury of suprascapular nerve at the spinoglenoid notch has been found to cause isolated atrophy and weakness of the infraspinatus muscle. This condition is also known as infraspinatus syndrome. A systematic literature review by Lee et al. (2007) found that suprascapular neuropathy due to infraspinatus syndrome is common in overhead game athletes, particularly volleyball players. (https://www.shoulderdoc.co.uk/article/1250)
Two main sites for suprascapular nerve injury are: the suprascapular notch and the spinoglenoid notch. The symptoms alongside clinical presentation for suprascapular neuropathy thus depend on the location of nerve injury. Injury of suprascapular nerve at the spinoglenoid notch has been found to cause isolated atrophy and weakness of the infraspinatus muscle. This condition is also known as infraspinatus syndrome. A systematic literature review by Lee et al. (2007) found that suprascapular neuropathy due to infraspinatus syndrome is common in overhead game athletes, particularly volleyball players. (https://www.shoulderdoc.co.uk/article/1250)
One important reason for traction injury in volleyball players is the huge amount of motion occurring at the shoulder during throwing action. The role of the scapula in allowing throwing motion as well as other overhead sports activity is now well-researched. It has been observed that the movement of the scapula during the protraction and retraction of hands leads to significant trauma of suprascapular nerve at both the suprascapular and spinoglenoid notches. This phenomenon is known as the ‘sling effect’. The sling effect proposes that certain positioning of upper limb during overhead activity exposes the suprascapular nerve at the suprascapular notch to a significant amount of sheer stress and thus injury. Sling effect also suggests that the suprascapular nerve is exposed to high risk of traction injury when it bends around the spine of the scapula at the spinoglenoid notch (Arash et al. 2015).

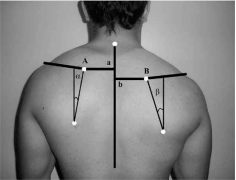 Chronic overuse of shoulder, as well as functional instability, may cause the suprascapular nerve to angle sharply at the spinoglenoid notch, as an adaptive response. This condition is known as ‘SICK scapula’ which is an abbreviation to Scapular protraction, Inferior border prominence, Coracoid tightness, and Kinesis abnormalities of the scapula (Burkhart et al. 2003). While imaging for the shoulder injuries of volleyball players, Crema & Murakami (2016) found that SICK scapula significantly contributes to increased tension on the suprascapular nerve and thus causes traumatic injury.
Chronic overuse of shoulder, as well as functional instability, may cause the suprascapular nerve to angle sharply at the spinoglenoid notch, as an adaptive response. This condition is known as ‘SICK scapula’ which is an abbreviation to Scapular protraction, Inferior border prominence, Coracoid tightness, and Kinesis abnormalities of the scapula (Burkhart et al. 2003). While imaging for the shoulder injuries of volleyball players, Crema & Murakami (2016) found that SICK scapula significantly contributes to increased tension on the suprascapular nerve and thus causes traumatic injury.
https://www.shoulderdoc.co.uk/article/930 http://www.scielo.br
The spinoglenoid ligament lays into the posterior glenohumeral capsule. Observations suggest that the ligament gets stretched and rigid with the abduction and internal rotation of the ipsilateral upper limb across the body. Such action leads to the traction of suprascapular nerve at the spinoglenoid notch (Crema & Murakani, 2016).
Sandow & Ilic (1998) provided another proposal for traumatic injury to the suprascapular nerve. According to them, when the upper limb is abducted and externally rotated, the medial border of the spinatus tendon present at the spinoglenoid notch compresses the suprascapular nerve. Repeated upper limb action thus causes trauma to the nerve and injures it. Plancher & Petterson (2016), recently supported this mechanism of nerve injury in their research paper.
The injury to the posterior part of the suprascapular nerve is thought to occur due to multiple, abrupt, peculiar stretching of infraspinatus tendon during the deceleration phase of the floater serve (the most common type of overhead volleyball serve). Ferretti observed such injury in volleyball players while Arash et al. (2016) observed this in various overhead sports players as well as labourers.
2.3 Other etiologies:
- Nerve compression: According to Raddic & Wallace (2016) direct compression of suprascapular nerve passing through spinoglenoid notch can occur due to ganglionic cysts arising from the glenohumeral joint. Such cysts are formed by synovial fluid leakage due to injury to the posterior glenoid labrum. Incidences of suprascapular nerve compression due to a bone tumor or the surrounding soft tissues are very rare but not absent.
- Nerve ischaemia: In very rare conditions, microemboli formed after any trauma gets trapped in the suprascapular artery and then migrate to the vasa nervorum thus hindering the blood and fluid supply to the suprascapular nerve. This leads to nerve ischemia and then neuropathy (Shin et al. 2016).
3. PRESENTATION & DIAGNOSIS OF SUPRASCAPULAR NEUROPATHY
The peculiar clinical presentations of suprascapular neuropathy are as follows:
- Shoulder pain which worsens on cross body abduction or internal rotation of ipsilateral muscle.
- Atrophy of supraspinatus or/and infraspinatus muscle, observable on physical examination.
- The weakness of ipsilateral shoulder abduction observed during manual muscle testing.
- The weakness of external rotation of shoulder observed during manual muscle testing.
- Pain elicited by pressure application over the suprascapular and spinoglenoid notch.
- The tenderness between the clavicle and the spine of the scapula or deep and posterior to the acromioclavicular joint (Podgorski et al. 2014).
Radiological examination using X-rays is the first step for diagnosis if suprascapular neuropathy is suspected. It is important to have a radiological view of a suprascapular notch and spinoglenoid notch along with a standard view of the shoulder area. However, no remarkable changes can be observed in the radiological images unless is a prominent trauma responsible for the condition. MRI of the shoulder helps in identifying muscle oedema, muscle atrophy, and ganglionic cyst, if present. These factors are responsible for suprascapular neuropathy due to direct compression. Three Tesla (3-T) MRI scan is another tool used in the diagnosis of suprascapular neuropathy as it helps to identify any nerve abnormality or any denervation changes in muscles. Ultrasound is also appliable for the diagnosis of cysts and other muscle abnormalities as it is an inexpensive and relatively accurate diagnostic tool (Ahlawat et al. 2015).
Electrodiagnostic studies are gaining increasing popularity as an important diagnostic tool for suprascapular neuropathy. Positive sharp waves and fibrillation potentials indicated by electromyography can suggest denervation while polyphasic motor unit action potentials suggest motor innervation abnormalities. Larisa et al (2014) suggest that electromyography (EMG) and nerve conduction velocity (NCV) tests are the gold standards for the detection of suprascapular nerve injury. EMG and NCV are suggested in the following conditions:
- Consistent pain on the back upper side of the shoulder and no confirm diagnosis is found.
- Atrophy as well as the weakness of supraspinatus and infraspinatus tendons in the absence of rotator cuff injury.
- MRI observations show muscle edema.
- Massive rotator cuff tendons with retraction and traction on the nerve.
There are published and examined normative values for electrodiagnostic studies. According to which, the normal distal motor latencies to the supraspinatus muscles during stimulation at the Erb point are 2.7 msec ± 0.5 and to the infraspinatus muscles, 3.3 msec ± 0.5. Side-to-side differences greater than 0.4 msec suggest focal entrapment of the SSN or another neural injury (Larisa et al. 2014).
In some cases, where outcomes of these electrodiagnostic studies are negative or not specific; fluoroscopically guided local anesthetic injection is used. This injection is administered to the region of suprascapular nerve and related pain relief is evaluated. This method is very effective in confirming the involvement of suprascapular nerve injury in shoulder pain (Debbie et al. 2014).
4. TREATMENT MODALITIES FOR SUPRASCAPULAR NEUROPATHY
Treatment for suprascapular neuropathy is selected on the basis of different factors like etiology of nerve damage, the severity of nerve damage, duration of pain and weakness in shoulder, degree of functional disability and patient’s choice. The three main types of treatment options are conservative physical therapy, nerve blocks and surgical repair.
4.1 Physical therapy:
If the suprascapular neuropathy is caused due to rotator cuff tear or labral tear with paralabral cyst, the treatment selection is done with regards to the pathology. However, in the case of isolated nerve injury, the conservative treatment plan including activity modification, analgesic drugs, and conservative physical therapy is initiated. The patient is asked to avoid or stop overhead activity as soon as he/she is diagnosed with suprascapular neuropathy. Following which, a physical therapy program is initiated which focuses on the movement of shoulder and muscle strengthening. The therapy also includes scapular stabilisation (Trojian, 2015).
Different studies on patients with isolated suprascapular neuropathy suggest that non operative treatment for 6 months to 1 year provides good to excellent outcomes in the majority of the patients while surgical intervention following physical therapy is required by only 20% patients (Lee et al. 2007). Boykin et al (2010) suggest that such non-operative treatments in the case of suprascapular neuropathy due to compression by mass or a cyst do not provide satisfactory results. It has been found that 53% of patients with suprascapular neuropathy due to spinoglenoid cyst get significant pain control and symptomatic relief with non-operative methods while 96% of such patients experienced positive outcomes with surgical treatment.
4.2 Surgical Treatment:
In case the conservative physical therapy for isolated suprascapular neuropathy fails, the patient is switched to surgical intervention. Furthermore, surgical intervention is immediately offered if suprascapular neuropathy is concomitant to rotator cuff tear or labrum tears with paralabral cysts. However, literature review suggests that there are debates about the application of surgical intervention for correcting nerve decompression in case of concomitant pathology. Many researchers recommend only for the correction of the isolated rotator cuff or labral repair and avoid surgery for nerve decompression (Boykin et al. 2010).
Nerve damage at the suprascapular notch is usually treated with the release of the transverse ligament by an open or arthroscopic technique. Fewer complications have been observed with the open technique. Patients are reported to have adequate pain management as well as improved muscle strength with the open technique. However, muscle atrophy cannot be reversed in all the cases using this technique. Improvement of supraspinatus muscle strength is observed among 90% of patients treated by open technique while no significant improvement of infraspinatus muscle is seen (Kim et al. 2005). While there are no specific indications for arthroscopic suprascapular nerve decompression, it has been found to be similarly effective in resolving pain. However, extensive data is not available to show the effectiveness of the technique in treating muscle atrophy and weakness (Boykin et al. 2010).
Nerve damage at spinoglenoid notch is usually secondary to nerve compression by the space-occupying lesion. Surgical management of such lesions often requires open or arthroscopic approach and resection of the lesion. It is noteworthy that patients with suprascapular neuropathy at spinoglenoid notch show poor results with physical therapy alone and thus are suggested to have surgical intervention immediately. Cyst recurrence rates are very low with both the methods (Petra et al. 2013). Literature review suggests that ultrasound-guided paralabral cyst aspiration is a good alternative to surgical intervention for suprascapular neuropathy due to compression at spinoglenoid notch. While the majority of patients reported excellent pain relief with the technique, recurrence rates for cyst are found to be between 75 – 100% (Moen et al. 2012).
4.3 Nerve Block:
Nerve blocks are non-surgical treatment options for suprascapular neuropathy. Nerve blocks are usually administered to manage shoulder pain in preoperative setups as well as in the case of painful shoulder conditions like adhesive capsulitis. Diagnostic usage and specificity of nerve blocks are widely debated, but the blocks are used to achieve rapid symptomatic relief so that the patient can properly participate in the rehabilitation physical therapy. Nerve blocks consist of an injection of an anaesthetic mixed with corticosteroid administered to the suprascapular notch (Blum et al. 2013).
Newer techniques like radiofrequency ablation of suprascapular nerve or palliative treatment for pain due to suprascapular neuropathy are still under consistent research phase and are not yet widely applied.
5. CONCLUSION
The incidences of suprascapular neuropathy can be more easily recognised now due to increased understanding of the condition and improved diagnostic methods. Overhead athletes presenting with vague posterosuperior shoulder pain, muscle atrophy, weakness of supraspinatus and infraspinatus tendons must be investigated for suprascapular neuropathy. The condition must also be investigated in all the athletes with rotator cuff tear, due to the high incidence. MRI and EMG are the most reliable diagnostic techniques to identify suprascapular neuropathy and rotator cuff health. Recently, fluoroscopically guided injections to the suprascapular notch are also gaining popularity as a diagnostic method for the condition. While conservative physical methods can be applied to treat the isolated suprascapular neuropathy, open or arthroscopic surgical corrections are compulsory to treat suprascapular neuropathy due to rotator cuff tear and cystic compression.
REFERENCES:
Ahlawat S, Wadhwa V, Belzberg AJ, Batra K, Chhabra A. (2015) Spectrum of suprascapular nerve lesions: normal and abnormal neuromuscular imaging appearances on 3-T MR neurography. AJR Am J Roentgenol. 204 (3), 589-601.
Arash A., Michael J., and Felix H. (2015) Suprascapular Nerve Release: General Principles. In: Elite Techniques in Shoulder Arthroscopy. Switzerland: Springer International Publishing, 271-281.
Blum A, Lecocq S, Louis M, Wassel J, Moisei A, Teixeira P. (2013) The nerves around the shoulder. Eur J Radiol., 82(1),2-16.
Boykin RE, Friedman DJ, Higgins LD, Warner JJ. (2010) Suprascapular neuropathy. J Bone Joint Surg Am., 92(13), 2348-64.
Burkhart SS, Morgan CD, Kibler WB. (2003) The disabled throwing shoulder: spectrum of pathology Part III: The SICK scapula, scapular dyskinesis, the kinetic chain, and rehabilitation. Arthroscopy, 19(6), 641-61.
Crema M., and Murakami A. (2016) Imaging of volleyball injuries. In: Imaging in Sports-Specific Musculoskeletal Injuries. Switzerland: Springer International Publishing, 663-695.
Cummins CA, Schneider DS. (2008) Peripheral nerve injuries in baseball players. Neurol Clin., 26(1), 195-215.
Debbie L., Angel M., William E., Susan V., and Ambrose J. (2014) Optimization and Standardization of Technique for Fluoroscopically Guided Suprascapular Nerve Blocks. American Journal of Roentgenology, 202(3), 576-584, 2014.
Gosk J, Urban M, Rutowski R. (2007) Entrapment of the suprascapular nerve: anatomy, etiology, diagnosis, treatment. Ortop Traumatol Rehabil, 9(1), 68-74.
Greiner K., Golser M, Wambacher F, Kralinger G, and Sperner T. (2003) The course of the suprascapular nerve in the supraspinatus fossa and its vulnerability in muscle advancement. Journal of Shoulder and Elbow Surgery, 12(3), 256-259.
Kim D, Murovic JA, Tiel R, and Kline D. (2005) Management and outcomes of 42 surgical suprascapular nerve injuries and entrapments. Neurosurgery, 57(1), 120-127, 2005.
Lajtai G, Pfirrmann CW, Aitzetmüller G, Pirkl C, Gerber C, and Jost B. (2009) The shoulders of professional beach volleyball players: high prevalence of infraspinatus muscle atrophy. The American Journal of Sports Medicine, 37(7), 1375-1383.
Larisa J., Elena J., Marisa J., and Jeffrey A. (2014) Evaluation, Treatment, and Outcomes of Suprascapular Neuropathy: A 5-Year Review. PM & R, 6(9), 774-80.
Lee BC, Yegappan M, Thiagarajan P. (2007) Suprascapular nerve neuropathy secondary to spinoglenoid notch ganglion cyst: case reports and review of literature. Ann Acad Med Singapore, 36(12),1032-5.
Lewis L., Michael T., Paul Y., and Jon J. (2012) Suprascapular Nerve: Is It Important in Cuff Pathology? Advances in Orthopedics, Article ID 516985.
Moen TC, Babatunde OM, Hsu SH, Ahmad CS, Levine WN. (2012) Suprascapular neuropathy: what does the literature show? J Shoulder Elbow Surg., 21(6), 835-46.
Petra M, Gaspar S, Sven L, Peter H, and Mathias W. (2013) Results of Arthroscopic Partial Repair of Large Retracted Rotator Cuff Tears. Arthroscopy-The Journal of Arthroscopic and Related Surgery, 29(8), 1275-1282, 2013.
Pillai G, Baynes JR, Gladstone J, Flatow EL. (2011) Greater strength increase with cyst decompression and SLAP repair than SLAP repair alone. Clin Orthop Relat Res., 469(4), 1056-60.
Plancher K., and Petterson S. (2016) Distal Suprascapular Nerve Compression: Spinoglenoid Ligament Release. In: Elite Techniques in Shoulder Arthroscopy. Switzerland: Springer International Publishing, 283-302.
Podgorski M, Miroslaw T, Marcin S, Piotr G, Ludomir S, and Michal P. (2014) New parameters describing morphological variations in the suprascapular notch region as potential predictors of suprascapular nerve entrapment. Bmc Musculoskeletal Disorders, 15.
Raddic R & Wallace A. (2016) Arthroscopic release and labral repair for bifocal compression of the suprascapular nerve. Shoulder & Elbow, 8(1), 32-36.
Trojian T. (2015, October 13) Suprascapular Neuropathy. Retrieved from: http://emedicine.medscape.com/article/92672-overview