Unusual Presentation of Intravascular Lymphomatosis
Intravascular lymphomatosis presenting as skin lesions and subacute encephalopathy
Intravascular lymphomatosis is a neoplastic multisystemic disease; it is a rare subtype of diffuse large cell lymphoma characterized by the presence of lymphoma cells in the lumina of small vessels. A 49-year-old Caucasian women was admitted to the Department of Internal Medicine for fatigue, night sweats, loss of weight, and multiple nodules in the forearms. Three months ago the patientï‚¢s family noticed problems with her cognitive function, she displayed difficulties with common daily tasks. The neurological examination revealed bradypsychia. Laboratory data showed modestly high levels of lactate dehydrogenase, and C-reactive protein. The day after admission, the patient had headache which raised in intensity; his mental status deteriorated, she was disoriented to time and place. She presented nucal rigidity. The CSF examination revealed a hemorrhagic aspect, elements 30/mm³, cytology: lymphocytes 90%, numerous erythrocytes, proteinorachia 96 mg/dL, glycorrachia 60 mg/dL. Intravenous Methylprednisolone (0.5 g two times a day) and Mannitol 20% 1g/kgw/day were administered for five days without response. She became comatose and she died six days after hospitalization. The post-mortem macroscopically brain examination showed a swallen brain, with diffuse hemorrhagic areas in the supratentorial subcortical regions. Microscopically examination showed capillaries, venules, and many arterioles distended by large malignant cells suggesting malignant lymphocytes which were intraluminal. Every organ was involved, except bone marrow and lymph nodes. Immunohistochemical studies showed intensive staining for B cells and negative staining for factor VIII related antigen, a specific endothelial cell marker. Intravascular lymphomatosis was the post-mortem diagnostic. It represents a difficult diagnostic challenge which involves laboratory, imagistic and immunohistochemical investigations.
Key words: intravascular lymphomatosis, subacute encephalopathy, skin lesions
Intravascular lymphomatosis is a neoplastic multisystemic disease; it is a rare subtype of diffuse large cell lymphoma characterized by the presence of lymphoma cells in the lumina of small vessels ï›1ï.
Clinical presentation is proteinaceous. Ante-mortem diagnosis is challenging and frequently impossible. Early diagnosis and treatment before disease dissemination is very difficult but increases survival and remission.
CASE PRESENTATION
We present the case of a 49-year-old right-handed Caucasian women who was admitted to the Department of Internal Medicine for fatigue, night sweats, loss of weight (10 kilograms in three months), and multiple nodules in the forearms. She had no previous medical history three months before admission. Three months ago the patientï‚¢s family noticed problems with her cognitive function, she displayed difficulties with common daily tasks. Multiple nodules were observed in the forearms. A neurological examination was normal, excepting bradypsychia.
Laboratory data, including blood cell counts and biochemistry were almost within normal limits, except for modestly high levels of lactate dehydrogenase (LDH 420 IU/L), and C-reactive protein (CRP 14 mg/L). The results of coagulation tests were normal.
The day after admission, the patient had headache which raised in intensity; over the next few days his mental status deteriorated, she was disoriented to time and place. She presented nucal rigidity. The electroencephalogramm revealed generalized delta-theta slowing.
The CSF examination revealed a hemorrhagic aspect, elements 30/mm³, cytology: lymphocytes 90%, numerous erythrocytes, proteinorachia 96 mg/dL, glycorrachia 60 mg/dL.
A contrast-enhanced CT of the chest, abdomen, and pelvis failed to reveal any abnormal lesions. The dermatologic examination recommended a skin biopsy, but the patientï‚¢s family did not agree with it.
Intravenous Methylprednisolone (0.5 g two times a day) and Mannitol 20% 1g/kgw/day were administered for five days without response. The patient became increasingly less responsive. The clinical course worsened by the development of an upper gastrointestinal bleed. She became comatose and she died six days after hospitalization before any specific treatment.
The post-mortem macroscopically brain examination showed a swallen brain, blood in the subarachnoid space, diffuse hemorrhagic areas in the supratentorial subcortical regions.
Microscopically examination showed capillaries, venules, and many arterioles distended by large malignant cells with nucleoli and eosinophilic cytoplasm, suggesting malignant lymphocytes (Figure 2 and Figure 3). The malignant cells were intraluminal.
Every organ was involved, except bone marrow and lymph nodes (Figure 4).
Immunohistochemical studies showed intensive staining for B cells (B-cell-associated antigens, such as CD20 and CD79a) (Figure 5-7) and negative staining for factor VIII related antigen, a specific endothelial cell marker (Figure 8).
The final diagnosis was established: Intravascular lymphomatosis
DISCUSSION
Intravascular lymphomatosis is regarded by the WHO as a rare subset of diffuse large B-cell lymphoma (DLBCL), characterized by the proliferation of atypical lymphoid cells in the lumina of small vessels in various organs with little or no involvement of the organ parenchima ï›1ï.
The disease was first described in 1959 by Pfleger and Tappeinner in Germany as ”angioendotheliomatosis proliferans systemisata”. It was described using many terms over the years: angioendotheliomatosis proliferans systemica, malignant angioendotheliomatosis, intravascular lymphomatosis, Kiel Classification: angio-endotheliotropic (intravascular) lymphoma, Lukes-Collins Classification: angiotropic large cell lymphoma, REAL Classification: diffuse large B-cell lymphoma (REAL-Revised European-American Lymphoma).
Intravascular large B-cell lymphoma (IVLBCL) is not defferent from B-IVL or T-OVL ina biologic sense and IVL seems to be better terminology than IVLBCL. It includes the T-cell phenotype that constitutes 9% of cases ï›2ï.
The disease involves several organs such as brain and skin, whereas spleen, lymph nodes and bone marrow are generally spared ï›3-5ï.
Recently, it has been suggested that intravascular lymphomatosis might have a predilection not only for the vessels but for both the central nervous system (CNS) and peripheral nervous system (PNS) ï›6, 7ï.
The predilection of the tumor cells for capillary endothelium is likely related to the expression of molecules on the surface of lymphocytes that allows for preferential binding within the vascular channel. Aberrant expression of CD11a and CD49d (VLA-4) on intravascular lymphomatosis cells has been proposed as a possible mechanism because these adhesion molecules would enable tumor cells to home CD54 (CD11a ligand) and CD106 (CD49d ligand), which are expressed on endothelial cell surface ï›8ï.
Another study demonstrated that intravascular lymphomatosis cells were consistently lacking in CD29 (ï¢1 integrin) and CD54 (ICAM-1), both of wich are regarded as essential for lymphocyte homing and transvascular migration ï›9ï.
Immunohistochemically, tumor cells usually express B-cell-associated antigens, such as CD19, CD20, CD22 and CD79a. Several cases have been reported to express CD5. A T-cell phenotype of intravascular lymphomatosis is reported in rare cases and have shown a coexpression of CD5 ï›1ï ï›8ï ï›10ï.
Clinical presentation are CNS involvement (some patients may also present with myopathy and peripheral neuropathy, cutaneous involvement, fever of unknown origin, and hemophagocytic syndrome ï›11, 12ï.
The neurologic symptoms consist in focal sensory and motor deficits, stroke-like episodes, generalized weakness, altered senzorium, rapidly progresive dementia, seizures, dysarthria, ataxia, vertigo, transient visual loss, peripheral neuropathy, polyradiculopathy, myopathy and myelopathy ï›13-29ï.
Neurological intravascular malignant lymphomatosis symptoms were divided in four groups: 1) progressive, multifocal cerebrovascular events, 2) spinal cord and nerve root vascular syndromes, 3) subacute encephalopathy, 4) peripheral or cranial neuropathies ï›13ï.
Initial diagnosis of stroke, encephalomyelitis, Guillain-Barré syndrome, vasculitis, and multiple sclerosis are often made, and the diagnosis of intravascular lymphomatosis is often not established until autopsy ï›14ï ï›30-33ï.
Brain MRI shows abnormalities, such as multiple, metachronous cortical or subcortical lesions that are hyperintense on T2-weighted and fluid-attenuated inversion recovery (FLAIR) images, suggestive of small vessel ischemia or demyelination. Cerebral imaging shows no characteristic features, but occlusive infarcts of multiple ages usually can be found. In some instances the disease can mimick vasculitis ï›15ï ï›34-36ï.
Diffusion-weighted images (DWI) lesions eighter vanished or followed the typical pattern of an ischemic small vessel stroke with evolution of abnormal FLAIR signal followed by enhancement with gadolinium in the subacute stage and tissue loss in the chronic stage; DWI and FLAIR abnormalities proved to be partially reversible, correlating with the response to chemotherapy ï›34ï.
Some authors have defined five patterns of abnormal MR imaging findings: 1) infarct-like lesions (hyperintense areas on T2W with diffusion restriction), 2) nonspecific white matter lesions (poorly margined hyperintense lesions on T2W without mass effector abnormal enhancement), 3) meningeal enhancement (abnormal enhancement along the surface of the cortex with a pia-arahnoid pattern extending>1 gyrus in>2 planes on postcontrast T1-weighted images.), 4) masslike lesions (intraparenchymal focal areas with contrast enhancement), and 5) hiperintense lesions in the pons on T2WI ï›38, 39ï.
The diagnosis may be provided by biopsies of the brain.
Macroscopically, the brain may show features of hemorrhage, thrombosis and necrosis.
Microscopically, the large tumor cells are localized in the lumina of small vessels and are characterized by vesicular nuclei and prominent nucleoli. Mitotic figures are frequently recognized. Malignant cells can only rarely be observed in the cerebrospinal fluid and the peripheral blood ï›40-42ï.
Cerebral biopsies may be falsely negative in neurological cases in which the diagnosis was confirmed post-mortem ï›43ï.
Intravascular lymphomatosis involvement of the skin consists in maculopapular eruptions, nodules, plaques, tumors, hyperpigmented patches, palpable purpura, ulcers, and infiltrating ”peau dï‚¢orange” and have been misdiagnosed as cellulitis, gangrene, vasculitis, squamous cell carcinoma, and Kaposiï‚¢s sarcoma ï›44ï.
Fever of unknown origin is seen in aproximately 45% of cases with intravascular lymphoma, the diagnosis was established by a random skin biopsy ï›45, 46ï.
The Asian variant of intravascular lymphomatosis is considered a hemophagocytic syndrome, characterised by fever, anemia, thrombocytopenia, and hepatosplenomegaly. There is involvement of reticuloendothelial system and the bone marrow ï›47-50ï.
Anemia, elevated lactate dehydrogenase, and elevated erythrocyte sedimentation rate are the most common laboratory abnormalities seen in intravascular lymphomathosis. Thrombocytopenia and leukopenia are seen less often.
PET scan may identify subclinical involvement ï›51ï.
Diagnosis work-up should include random nerve, muscle, skin, and other biopsies. Because diagnosis based on tissue other than skin is usually difficult in patients with suspected intravascular lymphomathosis, random skin bipsy should be considered even in patients with no evident skin lesions ï›52, 53ï.
The recommended treatment of intravascular lymphomathosis is a chemotherapy regimen such Cyclophosphamide, Doxorubicin (Hydroxydaunomycin), Vincristin (Oncovin), and Prednisone (CHOP) with the addition of the monoclonal antibody Rituximab (R-CHOP) in cases with a B-cell immunophenotype. Additional Methotrexate may be necessary to improve the outcome when there is CNS involvement. In case of refractory intravascular lymphomathosis a second line therapy can be performed followed by autologous bone marrow transplantation or autologous peripheral stem cell transplantation. Plasmapheresis has been discussed as providing temporary benefit ï›12ï ï›24ï ï›54-61ï.
In our case, clinical presentation of intravascular lymphomatosis was with skin lesions and subacute encephalopathy. The diagnosis was established post-mortem.
CONCLUSION
1) Intravascular lymphomatosis represents a difficult diagnostic challenge which involves laboratory, imagistic and immunohistochemical investigations.
2) Skin and sometimes brain biopsy is needed to establish the correct diagnosis.
Limfomatoza intravasculară este o afecÅ£iune neoplazică multisistemică; aceasta este un subtip rar de limfom difuz cu celule mari caracterizat prin prezenÅ£a celulelor limfomatoase în lumenul vaselor mici. O pacientă de rasă albă de 49 ani a fost internată în Clinica de Medicină Internă pentru astenie, transpiraÅ£ii nocturne, scădere ponderală ÅŸi multipli noduli la nivelul antebraÅ£elor. În urmă cu trei luni familia pacientei a observat probleme cognitive ÅŸi dificultăţi la îndeplinirea activităţilor cotidiene. Examinarea neurologică a relevat bradipsihie. Examenele de laborator au evidenÅ£iat valori moderat crescute ale lactat dehidrogenazei ÅŸi proteinei C reactive. A doua zi după internare pacienta a prezentat cefalee progresivă, starea mentală deteriorându-se ÅŸi redoare a cefei. Examenul LCR a relevat aspect hemoragic, 30 elemente/mm³, citologie: limfocite 90%, numeroase eritrocite, proteinorahie 96 mg/dl, glicorahie 60 mg/dl. S-au administrat metilprednisolon (0,5 g x 2 pe zi) ÅŸi manitol 20% 1g/kg/zi timp de cinci zile fără răspuns. Pacienta a prezentat stare de comă ÅŸi a decedat după ÅŸase zile de spitalizare. Examinarea cerebrală macroscopică post-mortem a relevat creier edemaÅ£iat cu zone hemoragice difuze la nivelul regiunilor subcorticale supratentoriale. Examinarea microscopică a evidenÅ£iat capilare, venule ÅŸi numeroase arteriole destinse de celule maligne mari sugerând limfocite maligne situate intraluminal. Toate organele erau afectate, cu excepÅ£ia măduvei osoase ÅŸi a ganglionilor limfatici. Studiile imunohistochimice au relevat marcare intensă pentru limfocitele B ÅŸi negativă pentru antigenul dependent de factorul VIII, marker specific al celulei endoteliale. Diagnosticul post-mortem a fost limfomatoză intravasculară. Acesta reprezintă o provocare diagnostică dificilă ce implică investigaÅ£ii de laborator, imagistice ÅŸi imunohistochimice.
Figure 1 Cerebral CT examination-multiple hyperdense supratentorial subcortical lesions
Figure 2 Cerebral intravascular lymphomatosis (H-E, OM x 100)
Figure 3 Cerebral intravascular lymphomatosis-a section stained immunohistochemically with an antibody to the CD20 marker, which stains B cells; positive rim of staining
Figure 4 Skin intravascular lymphomatosis-blood vessels are occluded and distended by a neoplastic lymphoid cells (H-E, OM x 200)
Figure 5 Cerebral intravascular lymphomatosis-a section stained immunohistochemically with an antibody to the CD79a marker, which stains B cells
Figure 6 Cerebral intravascular lymphomatosis-a section stained immunohistochemically with an antibody to the CD79a marker, which stains B cells (enlarged view)
Figure 7 Cerebral intravascular lymphomatosis-a section stained immunohistochemically with an antibody to the CD20 marker, which stains B cells (enlarged view)
Figure 8 Cerebral intravascular lymphomatosis-a section stained immunohistochemically with an antibody to the factor VIII marker, which stains the vessel wall
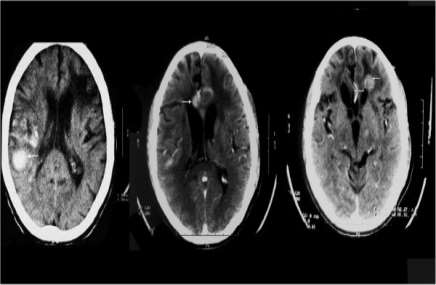
Figure 1 Cerebral CT examination-multiple hyperdense supratentorial subcortical lesions

Figure 2 Cerebral intravascular lymphomatosis (H-E, OM x 100)

Figure 3 Cerebral intravascular lymphomatosis-a section stained immunohistochemically with an antibody to the CD20 marker, which stains B cells; positive rim of staining

Figure 4 Skin intravascular lymphomatosis-blood vessels are occluded and distended by a neoplastic lymphoid cells (H-E, OM x 200)

Figure 5 Cerebral intravascular lymphomatosis-a section stained immunohistochemically with an antibody to the CD79a marker, which stains B cells

Figure 6 Cerebral intravascular lymphomatosis-a section stained immunohistochemically with an antibody to the CD79a marker, which stains B cells (enlarged view)

Figure 7 Cerebral intravascular lymphomatosis-a section stained immunohistochemically with an antibody to the CD20 marker, which stains B cells (enlarged view)

Figure 8 Cerebral intravascular lymphomatosis-a section stained immunohistochemically with an antibody to the factor VIII marker, which stains the vessel wall
Order Now