Historical Survey of Dental Restorative Materials
Historical Survey of Dental Restorative Materials
Introduction:
Dental restorative material is a biomaterial used to restore the shape and function of damaged or missing tooth (caused by caries or trauma).
Restorative materials can be divided into two types depending on whether they are designated to be applied directly to the injured tooth or fabricated in the lab firstly.
1. Direct Dental Restoration:
Direct restoration means the usage of dental materials to save injured tooth’s function. A filling is a way to restore a damaged tooth by decay to recover its function and shape again (1).
There are several kinds of materials which are used as filling. The right choice is determined by many factors; such as: extent of required repair, cost, having allergies to specific materials, etc…
Metallic Fillings:
- Gold fillings: gold has used as filling material. It is prepared in a laboratory and after that it is cemented into required place. Gold inlays are well compatible by gum tissues. Gold is considered the best filling material because it may last more than twenty years (1). However, gold filling often requires many visits to dentist as well as it is the most expensive choice. The following figure is for tooth with gold filling:

Fig. (1): Gold filling
- Amalgam Fillings: first introduction of amalgam was in the United States in 1830, then this material was developed in both England and France. The amalgam fillings consist of silver, copper, zinc, tin and mercury.
After starting of using amalgam as filling, controversy arose because of adding the mercury to fillings. At the beginning, this material is not embraced in the USA by the organized dentistry. In 1840, many members of dental surgeons of the American Society refused to use amalgam as filling material(2).
In fact, the amount of mercury which was added to fillings was harmful to the health of patients. The mercury exists in filling may seep into the patient’s system and lead to a number of health concerns, for example: cancers or multiple sclerosis. Therefore, nowadays a lots of precautions have been taken to be sure that amalgam fillings are safe as possible as for patients (3).
Generally, amalgam fillings are resistant to wear and inexpensive. But, according to their dark color, they are not desirable like other filling materials as well as they are not used in visible areas, like front teeth. The following figure is for tooth with amalgam filling:

Fig. (2):Amalgam filling
Non-metallic Fillings:
- Resin-Based Composite (RBC) fillings: composite fillings are closely to be the same color of natural teeth and these fillings are used where a natural appearance is required. The components are mixed and then placed directly into the tooth cavity, after that they harden. Actually, many experiences have approved that composites are not the ideal filling for large cavities because they may wear over time. As well, composites may become stained from tobacco or drinks like coffee or tea. They do not last more than three to ten years, however, recent research has suggested that the longevity of resin-based composites could be equally to amalgam (4). The following figure is for tooth with composite filling:

Fig. (3):Composite filling
- Porcelain fillings: these fillings could be inlays or onlays. They are produced to order in a dental laboratory and then bonded to the damaged tooth. Porcelain fillings can be resist staining and matched to the natural tooth color. Generally, porcelain restorations cover most of the tooth. However, the cost of these fillings is similar to gold fillings.
- Glass-ionomer cements/water-based cements: Self-setting which is pure glass ionomers, or light cured which is resin modified glass-ionomers. Glass ionomer restoratives become popular with dentists because of their adhesive properties as well their ease of handling. They are relatively poor in resistance to moisture. These fillings have adequate compressive strength to be used as core build-up. However, flexural strength and fracture toughness of these materials are low. Therefore glass ionomer cements are suitable to place where there is tooth substance remaining to support the filling material and where resistance could be obtained from tooth tissue. Cermet cements do not supply advantages more than glass ionomers and they usually have poor adhesion to tooth structure(5). In general, the longevity of glass-ionomers is lower than that of amalgam or RBCs (4).
- Long-term temporary fillings; for example: reinforced zinc oxide-eugenol cements (4).
2. Indirect Dental Restoration:
Indirect restorations are prepared in laboratory away from the injured tooth. Indirect restorations include inlays which are intracoronal, crowns and bridges that are extracoronal, or onlays which is considered as a combination of intracoronal- extracoronal.
Crowns:
Crowns could cover all/ partially the surfaces of tooth. After making a decision which restoration should be done for patient, materials and methods should be determined to begin the fabrication (5).
Design and Materials Selection for Indirect Restorations:
- Gold:
For more than 4 thousand years, gold has used as a restorative material in dentistry. The first gold fixed bridges were introduced by Romans and then its dental applications have published widely (6).
The selection of restoration type and design will depend on the clinical situation details. However, gold is considered as one of the most efficient restorative material especially as extracoronal. Fig 4,5 show Cast gold crown (7,8).

Fig (4): Cast gold crown

Fig (5): Cast gold crown
|
Advantages |
Disadvantages |
|
Having a hardness which is similar to the normal enamel |
Gold crown is fabricated by cast process from molten that may sometimes lead to microgaps at margins which are liable to decay |
|
Contours of occlusal and axial are built up clearly in the wax |
Visibly different from the color of natural teeth |
|
long-lasting |
High sensitivity hot/cold |
|
Used for complete/partial tooth coverage. |
long procedures for preparation (cast) and treatment |
|
Avoiding problems caused by using dissimilar metals |
High cost |
- Porcelain:
For many years, porcelain has used as a dental restorative material. Porcelain is a brittle material that requires special treatment for surface, such as: etching and silanisation.
Porcelain crowns require restriction to anterior teeth excluding some types such as, Empress II, Inceram and Procera which are considered high-strength ceramics.
|
Advantages |
Disadvantages |
|
Strong |
hardness of porcelain is more than natural enamel, that may cause damaging to the other natural teeth (for example; clench and grind) |
|
Natural looking |
Small thickness makes porcelain brittle and fracture |
|
No conductivity of (heat-cold) |
More reduction of tooth structure should be done |
|
Suitable for metal sensitivity-patients |
Fig 6 shows porcelain crowns (8).

Fig (6): porcelain crowns
- Porcelain – metal:
Porcelain – metal crowns combine between durability & strength of the metal, and good aesthetics of the porcelain, Fig.(7): shows porcelain – gold crown (8).

Fig (7): Porcelain – Gold Crown
|
Advantages |
Disadvantages |
|
Comparing with full porcelain it is Stronger & more durable |
Opacity because of the metal base |
|
Better aesthetic than full metal |
Existence of dark metal edge at the gum line |
|
Bonding techniques used are less sensitive than techniques used for full porcelain |
Porcelain and metal base could separate during use |
|
Limitation because of metal allergies of some Patients |
- Composites:
Recently, Composites are used widely in dentistry according to their high strength, high wear resistance and less expensive than other materials like: porcelain, gold, or zirconia. As well, composites used in onlay/crowns have permanent form stability comparing with other materials (5). However, sometimes a material “less wear-resistant” is more favorable to be sacrificial to nature. Fig. (8) shows a composite crown (5):

Fig (8):A composite crown
Table (1) illustrates comparison of materials used for indirect restoration (9):
table (1): Comparison of materials used for crown manufacturing
|
Porcelain |
Porcelain – metal |
Gold alloys |
Metal alloys |
||
|
Biocompatibility |
Well tolerated. |
some patients may show allergenic sensitivity to base metals. |
Well tolerated. |
Well tolerated, but some patients may show allergenic sensitivity to base metals. |
|
|
Esthetic |
natural color & translucency |
limits translucency because of metal. |
desirable color |
||
|
Durability |
Brittle & Strength is related to bond to underlying. |
strong & durable. |
High strength & toughness |
||
|
Fracture Resistance |
Weak under tension & impact. |
metal improve the strength. |
Highly resistant. |
||
|
Wear Resistance |
Highly resistant, except when porcelain surface becomes rough. |
Resistant |
|||
|
Sensitivity |
Low thermal conductivity |
High thermal conductivity |
|||
Implants:
First introduction of dental implants was in the 1960s by Brånemark. Dental implants are fabricated to replace missing teeth. The chemical and physical properties (composition & characteristics of the implant surface and its microstructure, in addition to the design of implant) determine the factors which influence the implant therapy. Many criteria should be achieved such as, strength, biocompatibility, toughness, resistance of wear, corrosion, and fracture. The design principles and the physical properties of the material must be compatible.
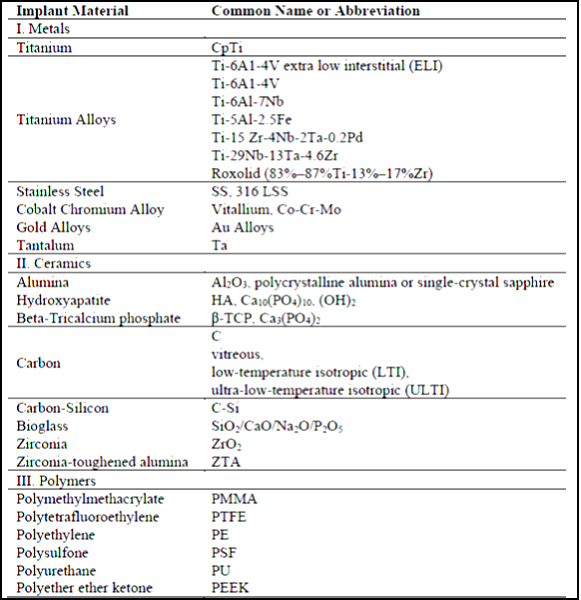
Table 2 includes materials used to produce dental implants due to their chemical composition (10).
Table (2): Chemical composition of implant material
- Titanium – Titanium Alloys:
Several metals and metallic alloys including: gold, cobalt chromium, and stainless steel are used to produce dental implants. Last research declare that titanium is the gold standard metal to fabricate dental implants. This material approves long-term survival during experiments (10) and totally inertia to fluids of the mouth (11).
Table (3): shows the mechanical and physical properties of biomedical titanium alloys.
Table (3): Mechanical and physical properties of biomedical titanium alloys
|
Material |
Modulus (GPa) |
Tensile Strength (MPa) |
Yield Strength (MPa) |
Elongation (%) |
Density (g/cc) |
Type of Alloy |
|
Cp Ti grade I |
102 |
240 |
170 |
24 |
4.5 |
α |
|
Cp Ti grade II |
102 |
345 |
275 |
20 |
4.5 |
α |
|
Cp Ti grade III |
102 |
450 |
380 |
18 |
4.5 |
α |
|
Cp Ti grade IV |
104 |
550 |
483 |
15 |
4.5 |
α |
|
Ti-6Al-4V- ELI |
113 |
860 |
795 |
10 |
4.4 |
α + β |
|
Ti-6Al-4V |
113 |
930 |
860 |
10 |
4.4 |
α + β |
|
Ti-6Al-7Nb |
114 |
900-1050 |
880-950 |
8-15 |
4.4 |
α + β |
|
Ti-5Al-2.5Fe |
112 |
1020 |
895 |
15 |
4.4 |
α + β |
|
Ti-15Zr-4Nb-2Ta-0.2Pd |
94-99 |
715-919 |
693-806 |
18-28 |
4.4 |
α + β |
|
Ti-29Nb-13Ta-4.6Zr |
80 |
911 |
864 |
13.2 |
4.4 |
β |
The α + β alloy is the most commonly used for the manufacturing of dental implants. This alloy is made up of 6% aluminum & 4% vanadium (Ti-6Al-4V) (10).
Reports indicate that incidence ranging of titanium implant fracture from 0% to 6%,on the other hand, it is an uncommon occurrence. Fig (9): shows the titanium implant fracture.
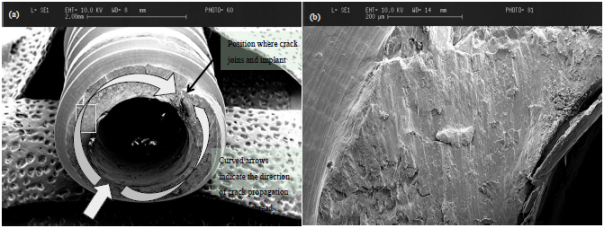
Fig (9): Titanium implant fracture.
Recently, there are some concerns that titanium could evoke an undesirable host reaction; however, little evidence is available about that.
- Ceramics
First introduction of ceramics to dental implants were in the form of coatings onto metal-based implants. They were used to improve osseointegration. Recently, various forms of ceramic coatings have been used for dental implants.
Table 4 illustrates ceramic materials used as dental implants (10):
Table 4: Ceramic materials used as dental implants
|
Material |
Chemical Composition |
|
Hydroxylapatite (HA) |
Ca10(PO4)6(OH)2 |
|
Tricalcium phosphate (TCP) |
α, β,Ca3(PO4)2 |
|
Fluorapatite (FA) |
Ca10(PO4)6F2 |
|
Tetracalcium phosphate |
Ca4P2O9 |
|
Calcium pyrophosphate |
Ca4P2O7 |
|
Brushite |
CaHPO4, CaHPO4·2H2O |
|
Bioglasses |
SiO2-CaO-Na2O-P205-MgO, |
|
Aluminium oxide |
Al2O3 |
|
Zirconium oxide |
ZrO2 |
Zirconia is the most favorable among oxide ceramics according to its excellent mechanical properties. Yttria stabilised tetragonal zirconia polycrystalline (Y-TZP) materials exhibits high corrosion & wear resistance, in addition to its high flexural strength (800 to 1000 MPa) comparing with other dental ceramics (10).
An understanding of the bio-mechanical failure modes of zirconia implants is essential so that an optimal zirconia implant design can be developed. Based on more fundamental studies in the biomaterials science field, the physical mechanism of ceramic implant failure can be either chemical and/or mechanical in nature. Mechanical failure can occur either during the surgical placement of the implant or subsequent functional loading.
Clinical examples of fracture modes of zirconia implants are shown in fig. 10,11:

Fig (10): zirconia implant fractured during surgery

Fig (11): zirconia implant fractured after loading.
References:
1. Colgate. Oral Care Centre, 2016. Weblog.
Available from:
http://www.colgate.com/en/us/oc/oral-health/procedures/fillings/article/what-is-a-filling
2. WOLFE B. Energetic Healthcare and Dentistry. Weblog.
Available from:
http://www.drwolfe.com/dentistry/mercury_fillings
3. The 123 Community Dentist Network. The History of Dental Fillings, 2013. Weblog.
Available from:
4. Report of the meeting convened at World Health Organization. Future Use of Materials for Dental Restoration. Switzerland, 2009.
5.. Restoration of teeth (complex restorations)
6. KNOSP H., HOLLIDAY R. J., CORTI C.W..”Gold in Dentistry: Alloys, Uses and Performance”,2003.
7. Donaldson J. A. “The Use of Gold in Dentistry”, AN HISTORICAL OVERVIEW. PART I, 1980.
8. RICH M.”A Comparison of Dental Crown Materials”. Health Centered Dentistry. Weblog.
Available from:
http://drmartharich.com/resources/a-comparison-of-dental-crown-materials
9.American Dental Association. Oral Health Topics- Dental Materials. Weblog.
Available from:
http://www.ada.org/en/member-center/oral-health-topics/dental-materials
10. OSMAN R. B., SWAIN M. V. “A Critical Review of Dental Implant Materials with an Emphasis on Titanium versus Zirconia”, 2015.
11. CROITORU S. M., MIHAILESCU I. N., POPOVICI I. A. “Materials and Technologies Used in Present Dental Implants Manufacturing”, 2014.